Opioid Dosing Calculator for Renal Failure
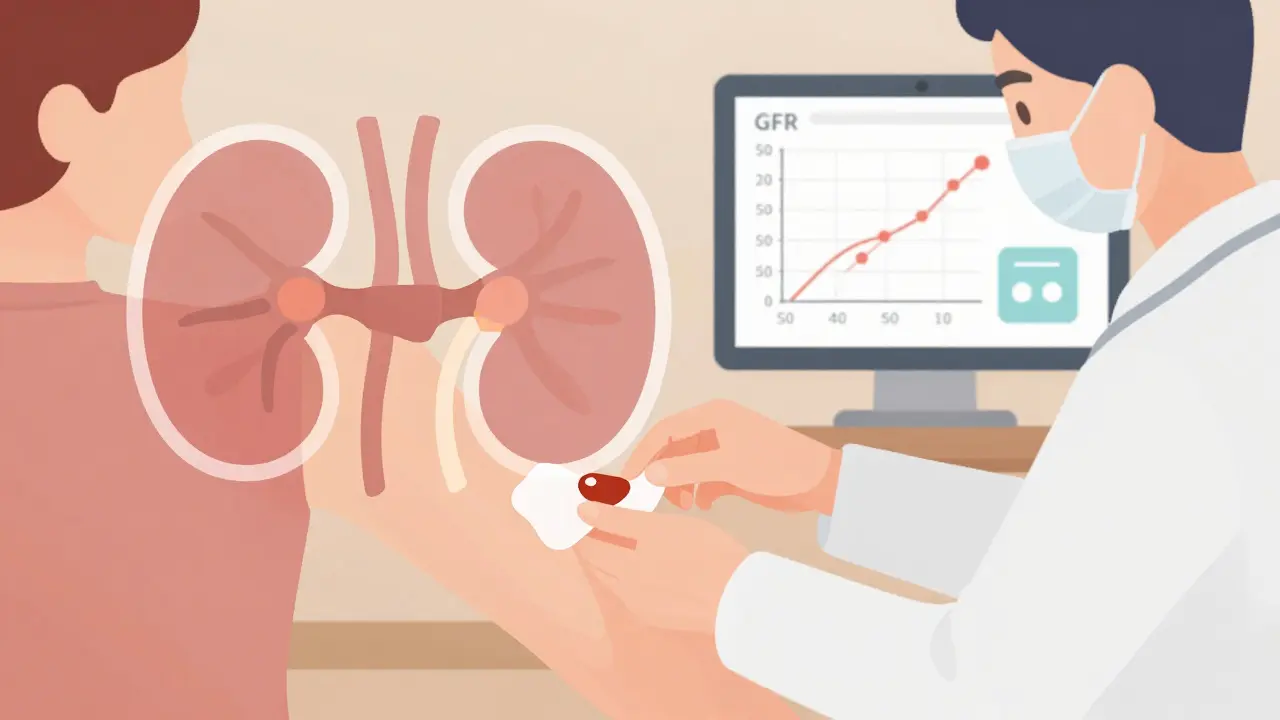
This tool helps healthcare providers calculate appropriate opioid dosages for patients with chronic kidney disease based on glomerular filtration rate (GFR). Always consider individual patient factors and consult full clinical guidelines.
Dosing Recommendations
When someone has advanced kidney disease, managing chronic pain becomes a tightrope walk. Opioids can help, but the wrong choice or dose can lead to seizures, confusion, or even respiratory failure. This isn’t theoretical - it’s happening in clinics every day. Up to 85% of people with end-stage renal disease (ESRD) suffer from moderate to severe pain, yet most don’t get adequate relief because doctors fear toxicity. The problem isn’t pain itself. It’s that most opioids and their metabolites build up in the body when kidneys can’t clear them. The result? Neurotoxicity. That’s why choosing the right opioid - and dosing it correctly - isn’t just important. It’s life-saving.
Why Standard Opioid Doses Are Dangerous in Kidney Failure
Most opioids are broken down in the liver and cleared by the kidneys. In someone with a glomerular filtration rate (GFR) below 30 mL/min, that clearance slows to a crawl. Morphine, for example, turns into morphine-3-glucuronide, a metabolite that doesn’t just hang around - it attacks the nervous system. People on morphine with severe kidney disease report muscle twitching, hallucinations, and seizures. Codeine is even worse. It turns into morphine in the body, and that metabolite accumulates fast. That’s why both are contraindicated in moderate to severe chronic kidney disease (CKD).
Meperidine (pethidine) is a hard no. Its metabolite, normeperidine, builds up at levels as low as 0.6 mg/L and causes violent seizures. It’s been banned in CKD patients for over a decade, but some prescribers still reach for it out of habit. Propoxyphene, another old-school opioid, was pulled from the market for good reason - it’s toxic in renal failure.
Even hydromorphone, often thought of as a safer alternative, has a hidden risk. Its metabolite, hydromorphone-3-glucuronide, accumulates in non-dialysis patients and increases neurotoxicity risk by 37% compared to those on dialysis. That’s why you can’t just reduce the dose - you have to understand the metabolite profile.
The Safest Opioids for Kidney Patients
Not all opioids are created equal. The safest options are those that rely mostly on liver metabolism and have minimal kidney clearance. Two stand out: fentanyl and buprenorphine.
Fentanyl is 85% metabolized by the liver. Only 7% is excreted unchanged by the kidneys. That makes it one of the few opioids that can be used safely in patients with GFR under 10 mL/min. Transdermal patches are ideal because they deliver steady levels without peaks and troughs. But here’s the catch: never start a fentanyl patch in someone who’s never taken opioids before. The risk of overdose is real. Patches are for chronic, stable pain - not acute flares.
Buprenorphine is another top choice. About 30% of it is cleared by the kidneys, but its metabolites aren’t neurotoxic. Studies show it can be used in dialysis patients without dose changes. It’s also less likely to cause respiratory depression than other opioids. The downside? It can prolong the QT interval on an ECG. That’s not a dealbreaker, but it means you need to check the patient’s heart rhythm before starting and after any dose increase.
Methadone is trickier. It’s metabolized by the liver and doesn’t form toxic metabolites, so it’s often used in CKD. But it’s a high-risk drug. It can cause fatal arrhythmias, especially in patients with electrolyte imbalances - common in kidney disease. You need ECG monitoring at initiation and after each dose change. In Canada and the U.S., prescribers need special licensing to use methadone for pain, not just addiction.
Dosing by Kidney Function: A Practical Guide
There’s no one-size-fits-all dose. It depends on your GFR. Here’s what works in real-world practice, based on KDIGO and clinical reviews:
- GFR >50 mL/min/1.73m²: Use full standard doses of fentanyl, methadone, or buprenorphine. Morphine is still risky - avoid it.
- GFR 10-50 mL/min/1.73m²: Reduce morphine to 50-75% of usual dose. Fentanyl can stay at 75-100%. Methadone and buprenorphine don’t need adjustment.
- GFR <10 mL/min/1.73m²: Morphine drops to 25% of usual. Methadone to 50-75%. Fentanyl to 50%. Buprenorphine remains unchanged.
For patients on hemodialysis, timing matters. Fentanyl isn’t recommended during dialysis because clearance is unpredictable. Buprenorphine is fine - it’s not removed by dialysis. Methadone can be given after dialysis, but monitor closely for sedation.
What About Newer Opioids Like Tapentadol?
Tapentadol is a newer option with a dual mechanism - it works on mu-opioid receptors and norepinephrine reuptake. It’s appealing because it doesn’t require dose adjustment in mild-to-moderate CKD (CrCl ≥30 mL/min). But there’s no data for ESRD. Until studies prove it’s safe in dialysis patients, stick with fentanyl or buprenorphine.
There’s also oxycodone. It’s used often, but 45% of its metabolites are cleared by the kidneys. Some clinicians use it at max daily doses of 20 mg for CrCl under 30 mL/min, but it’s not ideal. Hydromorphone, as mentioned, carries neurotoxicity risk. Avoid it unless you’re prepared to monitor for tremors or confusion.
Non-Opioid Alternatives and Complementary Strategies
Even the safest opioids carry risks. That’s why multimodal pain control is the gold standard. Gabapentin and pregabalin are commonly used for neuropathic pain in CKD, but they need serious dose reductions. Gabapentin: 200-700 mg once daily for CrCl under 30 mL/min. Pregabalin: half the usual dose, given every 24-48 hours. Both can cause dizziness and swelling - common in kidney patients already dealing with fluid overload.
Tricyclic antidepressants like nortriptyline are risky too. They can cause dangerous heart rhythms when potassium or magnesium levels swing. Serum levels above 100 ng/mL increase cardiac event risk by 2.3 times. Use them only if other options fail, and check levels regularly.
For opioid-induced constipation - which affects up to 80% of patients - naldemedine is the best choice. Unlike other laxatives or peripherally-acting opioid blockers, it doesn’t need dose adjustment in CKD or dialysis. Standard dose: 0.2 mg daily.
What Clinicians Are Doing Right - and Wrong
A 2022 survey found that 78% of nephrology practices use fentanyl patches as first-line for non-dialysis CKD patients. That’s good. But only 12% of CKD patients with chronic pain get guideline-concordant care. Why? Because most opioid labels don’t include renal dosing. A 2019 FDA review found 68% of opioid package inserts have no guidance for kidney disease. That forces doctors to guess.
Some hospitals, like Kaiser Permanente, have solved this by embedding renal dosing alerts into their electronic health records. Since 2018, they’ve cut inappropriate opioid prescriptions in CKD patients by 47%. That’s the kind of system change that saves lives.
Meanwhile, research is moving forward. The NIDDK’s PAIN-CKD study, launched in 2021, is tracking 1,200 patients over five years to see which opioid regimens lead to better outcomes. Early signs point to personalized medicine: CYP2D6 poor metabolizers have a 3.2-fold higher risk of morphine toxicity in CKD. Future guidelines will likely include genetic testing.
Bottom Line: What to Do Today
If you’re managing pain in a patient with CKD:
- Stop morphine and codeine. They’re not safe.
- Avoid meperidine and propoxyphene - never use them.
- For severe pain, start with transdermal fentanyl or buprenorphine.
- Use half the usual dose if GFR is under 15 mL/min.
- Check ECG before starting methadone or buprenorphine.
- Use naldemedine for constipation - no dose adjustment needed.
- Combine with non-opioid options: acetaminophen (safe in CKD), low-dose gabapentin, or physical therapy.
Pain is real. But so is the risk of harm. The goal isn’t to avoid opioids entirely. It’s to use them wisely. With the right drug, the right dose, and constant monitoring, patients with kidney failure can live with less pain - and more safety.
Can I use morphine for pain in kidney failure?
No. Morphine is contraindicated in moderate to severe chronic kidney disease (CKD) because its metabolite, morphine-3-glucuronide, accumulates and causes neurotoxicity - including seizures, myoclonus, and confusion. Even with dose reductions, the risk remains high. Safer alternatives like fentanyl or buprenorphine should be used instead.
Is fentanyl safe for patients on dialysis?
Fentanyl patches are generally safe for patients with advanced CKD, but they are not recommended during hemodialysis sessions. Dialysis can unpredictably clear fentanyl, leading to either inadequate pain control or sudden withdrawal. If a patient is on dialysis, use fentanyl between sessions and monitor closely. Buprenorphine is often preferred for dialysis patients because it’s not removed by the process.
What’s the best opioid for someone with ESRD on dialysis?
Buprenorphine is often the top choice for end-stage renal disease (ESRD) patients on dialysis. It’s not significantly removed by dialysis, its metabolites aren’t neurotoxic, and it doesn’t require dose adjustments. Fentanyl patches can be used between dialysis sessions, but not during. Methadone is an option but requires ECG monitoring due to QT prolongation risk.
Do I need to adjust opioid doses if a patient has a GFR of 20 mL/min?
Yes. A GFR of 20 mL/min indicates stage 4 CKD. For morphine, reduce the dose to 50-75% of the usual amount. Fentanyl can be used at 75-100% of standard dose. Methadone and buprenorphine typically don’t need adjustment. Always start low and titrate slowly, checking for sedation or confusion every 24-48 hours.
Why is meperidine (pethidine) so dangerous in kidney disease?
Meperidine breaks down into normeperidine, a metabolite that builds up in kidney failure. At serum levels above 0.6 mg/L, it causes severe neurotoxicity - including tremors, agitation, and life-threatening seizures. It has no safe dose in CKD and is strictly contraindicated in all stages of kidney disease, including dialysis patients.





Donna Packard December 17, 2025
This is such an important post. I’ve seen too many patients suffer because doctors defaulted to morphine without thinking about metabolites. It’s not just about pain control-it’s about not turning relief into a nightmare.
Thank you for laying this out so clearly.
Patrick A. Ck. Trip December 19, 2025
While I agree with the general gist, I must note that fentanyl patches are not always reliable in cachectic or hypothermic patients-skin perfusion matters. Also, typo: 'GFR ' should be 'GFR <10 mL/min'-I assume that’s what was meant.
Sam Clark December 20, 2025
As a nephrologist with 18 years in clinical practice, I can confirm that buprenorphine has become my go-to for CKD patients with chronic pain. The data supports its safety, and the risk-benefit profile is superior to nearly all alternatives.
That said, QT monitoring is non-negotiable. I’ve seen one case of torsades after a rapid titration-avoidable with proper protocol.
Jessica Salgado December 20, 2025
I’m a nurse who works in dialysis. Last week, a patient on morphine started hallucinating at 2 AM-screaming about spiders crawling on the ceiling. We had to stop it cold. He cried because he was in pain but couldn’t sleep. This post? It’s the kind of thing that should be printed and hung in every ER and nephrology clinic.
Why do we still teach morphine as first-line? It’s like prescribing arsenic for a headache.
Chris Van Horn December 21, 2025
Oh please. You're recommending fentanyl like it's some miracle drug? Have you ever seen someone on a patch overdose because they were 'just cold'? And buprenorphine? That's just suboxone for pain now? You're just pushing Big Pharma's agenda. Methadone is cheaper, more effective, and if you're scared of arrhythmias, maybe you're not cut out for nephrology.
Virginia Seitz December 23, 2025
Thank you!! 🙏 I’ve been telling my doc for months not to give my dad morphine. He’s on dialysis. Now I have something to show him. 💪
amanda s December 23, 2025
Who let this post go live? This is why America’s healthcare is broken-overcomplicating simple things. Just give them hydromorphone. Everyone knows it works. Stop being so cautious. We’re losing people to pain, not overdoses.
Peter Ronai December 25, 2025
Let me guess-you got this from a 2019 KDIGO guideline and think you’re the first person to ever understand renal pharmacology? I’ve been using buprenorphine since 2007. Also, you missed the point about meperidine’s half-life in anuric patients. And why no mention of oxycodone? It’s not perfect, but it’s not banned. You’re being dangerously incomplete.
Steven Lavoie December 26, 2025
Excellent summary. I appreciate how you distinguished between dialysis and non-dialysis patients. That’s a gap I see in so many residency handouts.
One thing I’d add: when switching from morphine to fentanyl, always allow for a 24-48 hour washout. The cross-titration window matters more than the dose itself.
Michael Whitaker December 27, 2025
It’s amusing how everyone treats this like it’s groundbreaking. In Europe, we’ve been using buprenorphine as first-line for CKD pain since the early 2000s. Here, we’re still debating whether to use morphine at all. The U.S. medical system is stuck in a time capsule.
Brooks Beveridge December 28, 2025
For anyone struggling with this in practice-start small. Buprenorphine 0.2 mg SL twice daily. Wait 3 days. Then go to 0.3 mg. Most patients don’t need more than 0.6 mg/day. It’s not a race to maximum dose. It’s about steady comfort.
And yes-your patient’s pain is real. Even if they don’t cry out. Even if they smile through it. That doesn’t mean it’s not there.
Anu radha December 29, 2025
My mother is on dialysis. She has back pain. Doctor gave her tramadol. She got dizzy and fell. I didn’t know what to do. Now I understand. Thank you.
Jigar shah December 30, 2025
Is there any data comparing the cost-effectiveness of fentanyl patches versus buprenorphine in low-income populations? The patch is expensive, and many patients can’t afford it even with insurance.
Sachin Bhorde December 31, 2025
Yo, this is solid. Fentanyl and buprenorphine are the real MVPs here. But don’t sleep on oxymorphone-it’s hepatically cleared, low renal excretion, and in my unit, we’ve had zero neurotox cases with it in CKD 4/5. Just titrate slow. And yeah, methadone? Only if you’ve got a cardiologist on speed dial. 🚨
Joe Bartlett December 31, 2025
Why not just use NSAIDs? They’re cheaper, safer, and work fine for most. Opioids are overused everywhere.