What Specific IgE Testing Actually Measures
Specific IgE testing looks for antibodies in your blood that react to particular allergens. These antibodies, called immunoglobulin E (IgE), are your body’s alarm system for things it thinks are dangerous - like peanuts, pollen, or cat dander. When you’re allergic, your immune system overreacts, producing IgE antibodies that trigger symptoms like sneezing, hives, or even anaphylaxis. This test doesn’t tell you if you feel allergic. It tells you if your blood has the exact antibodies that match a specific trigger.
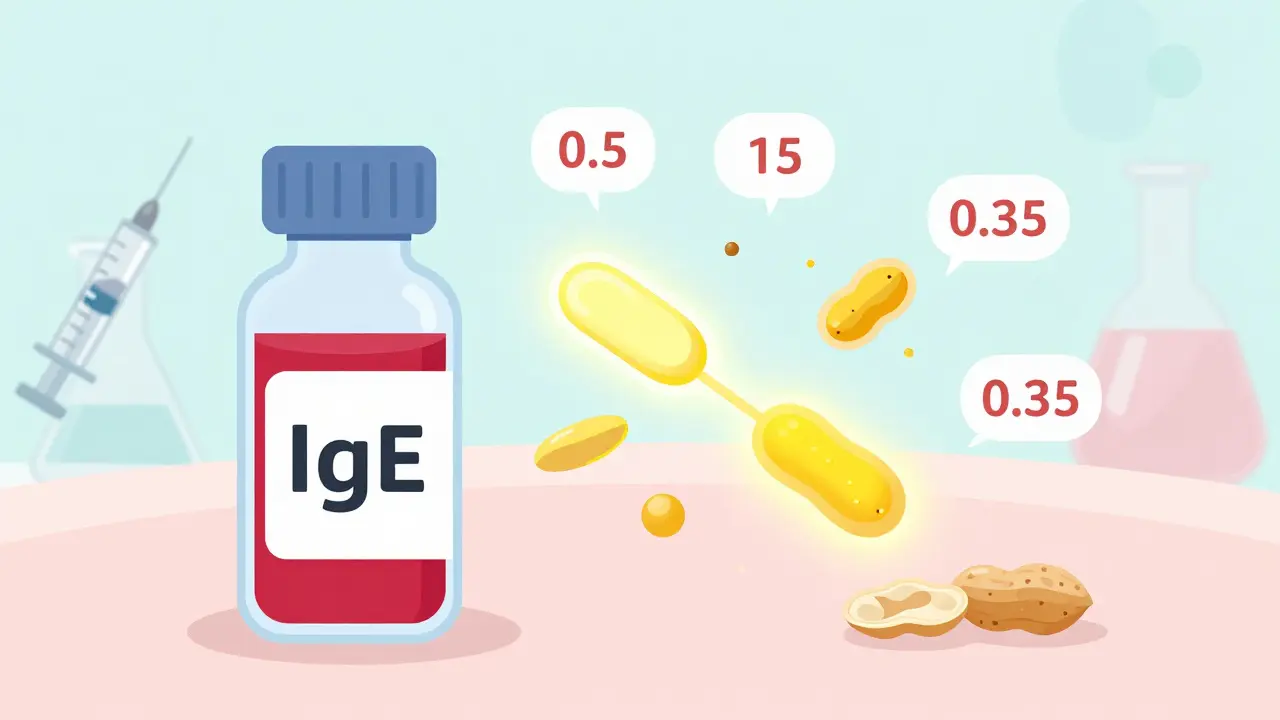
Back in the 1970s, doctors used a method called RAST, which gave only a yes-or-no answer. Today, the gold standard is ImmunoCAP a highly sensitive blood test that measures IgE levels in kUA/L units. It doesn’t just say "you’re allergic" - it tells you how much IgE is present. That number matters. A result of 0.5 kUA/L is very different from 15 kUA/L, even though both are above the normal cutoff.
How the Test Works and What You Need to Know Before It
There’s no special prep needed. You don’t have to stop your antihistamines. No needles in your skin. Just a standard blood draw - about 2 mL of serum in a yellow-top tube. The sample goes to a lab where it’s mixed with tiny particles coated with allergens. If your blood has IgE antibodies for that allergen, they stick. Then, a fluorescent dye lights up the match, and the machine counts how much light is emitted. That’s how they get your kUA/L number.
Unlike skin prick tests, which show immediate reactions on your skin, this test only measures what’s floating in your blood. That’s why it’s used when skin testing isn’t possible - like if you have severe eczema covering half your body, or if you’re on meds like antidepressants that block skin reactions. In fact, about 27% of pediatric patients get this test because they can’t stop their antihistamines for the 3-5 days skin testing requires.
Understanding Your Results: Numbers, Not Just Labels
Your report will show a number: 0.1, 0.8, 3.2, 18.5 - all measured in kUA/L. The standard cutoff for "positive" is 0.35 kUA/L. But here’s the catch: that number alone doesn’t tell you if you’ll react.
A result of 0.5 kUA/L might mean nothing if your total IgE is 100 kUA/L. But if your total IgE is only 2 kUA/L, that same 0.5 kUA/L could be a big red flag. That’s why labs now automatically check your total IgE when a specific IgE comes back positive. Without context, you’re guessing.
For peanut allergy, the data is clear: at 0.35 kUA/L, your chance of a real reaction is about 50%. At 15 kUA/L, it jumps to 95%. That’s why doctors don’t just look at "positive" or "negative." They look at the trend. High numbers mean higher risk. Low numbers? Often just sensitization - your body noticed the allergen, but you’ve eaten it 100 times without trouble.
Why You Shouldn’t Get a "Panel" of 20 Allergens
Some clinics offer "allergy panels" - 10, 20, even 30 allergens in one test. Don’t do it. The National Guideline for Laboratory Testing (2025) says this is a trap. When you test for too many things, you get false positives. Statistically, if you test for 20 allergens, you’re likely to get 1-2 random positive results even if you’re not allergic. That’s not science - that’s noise.
One study found that 60% of people who got 20+ allergen tests had at least one false positive. That leads to unnecessary food avoidance, anxiety, and even misdiagnosis. The guideline limits requests to 12 tests unless there’s clear clinical reason. If you’ve never had a reaction to shellfish, don’t test for it. If you’ve eaten eggs every Sunday for 10 years without issue, don’t test for egg. Only test for things you’ve reacted to - or things your doctor suspects based on your history.

What Tests Are Actually Recommended
Forget food mixes. Testing for "nut mix" or "dairy mix" is outdated and unreliable. Studies show false positive and false negative rates above 30%. That’s worse than flipping a coin. Instead, test for individual allergens: peanut, milk, egg, birch pollen, house dust mite.
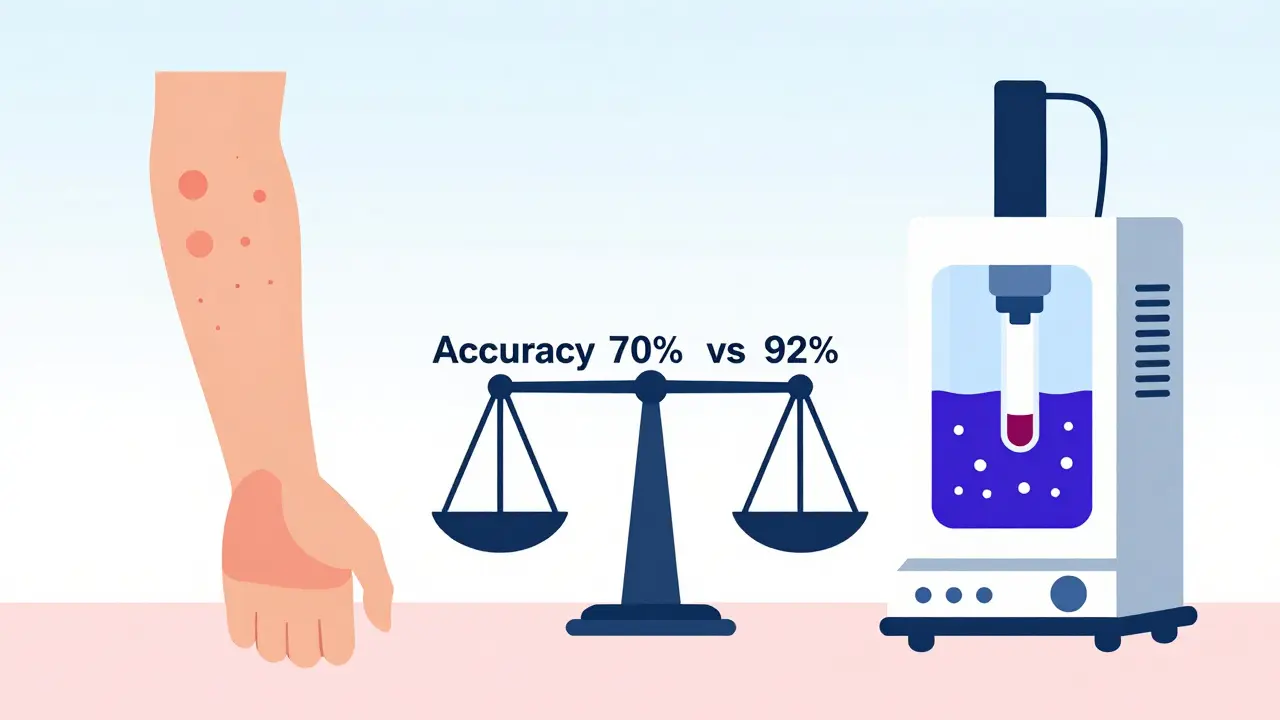
Even better, some labs now offer component-resolved diagnostics. Instead of testing for "cashew," they test for specific proteins like Ana o 3. This can tell you if you’re truly allergic to cashew - or just reacting because you’re also allergic to birch pollen (a common cross-reaction). This method boosts accuracy from 70% to 92%.
For most people, though, standard individual testing is enough. You don’t need 112 components. That’s what the ImmunoSolid Phase Allergen Chip (ISAC) does - but it’s only used in specialized allergy centers because interpreting the results requires expert training.
When to Use This Test - And When Not To
Use specific IgE testing when:
- You’ve had a clear reaction to a food or airborne allergen
- You can’t stop antihistamines for skin testing
- You have severe eczema or skin conditions that make skin testing unsafe
- Your doctor wants to confirm a suspected allergy before starting immunotherapy
Don’t use it when:
- You’re just curious about "what you might be allergic to"
- You’ve never had a reaction to something
- You’re testing for something you know you eat safely
- You’re looking for answers to chronic fatigue, headaches, or bloating - those aren’t IgE-mediated
Dr. Robert Boyle from Imperial College London says it best: "Only test when the result will change what you do." In primary care, 22% of IgE tests are unnecessary. That’s a waste of time, money, and emotional energy.
How Results Compare to Skin Testing
Skin prick testing is still the first choice for most allergists. It’s faster, cheaper, and shows real-time reactions. It’s also about 15-20% more sensitive for common allergens like pollen and dust mites. But it’s not perfect. If your skin is inflamed, or you’re on meds, it won’t work.
Specific IgE testing doesn’t replace skin testing - it complements it. Think of it as a backup plan. If skin testing isn’t possible, IgE testing gives you reliable data. If skin testing shows a reaction but you’re unsure if it’s clinically relevant, IgE levels help confirm the risk.
Both tests need interpretation. A 3mm wheal on skin or a 0.5 kUA/L in blood doesn’t automatically mean you’ll get sick. Your history is the key. Did you eat the food and break out in hives 10 minutes later? That’s real. Did you test positive for shrimp but eat it every holiday without issue? That’s not a true allergy.
Turnaround Time, Cost, and What to Expect
Most labs process specific IgE tests daily. Results usually come back in 3 business days. If your doctor orders something rare - like a seafood component or a tropical pollen - it might need to go to a specialized lab, which can take 5-7 days. There’s no rush. This isn’t an emergency test. Over 98% of orders are for diagnostic clarity, not acute care.
Cost varies by country and insurance, but it’s typically not covered unless there’s a documented history of allergic reaction. In Australia, Medicare may cover part of it if referred by a specialist. Private labs charge between $50-$150 per allergen. A single test is affordable. A 10-panel? That’s $500-$1,500. And as we’ve seen - it’s often misleading.
What Happens After You Get Your Results
Don’t panic. Don’t throw out your pantry. Don’t start avoiding everything on the list. Your allergist or doctor will look at your numbers with your history. If you have a high IgE level for peanut and you’ve had a life-threatening reaction, you’ll likely be given an epinephrine auto-injector and advised to avoid peanuts strictly.
If your IgE is low and you’ve eaten the food safely before? You’ll probably be told to keep eating it. Many people with low-level IgE sensitization never develop full-blown allergies. Avoiding food unnecessarily can actually increase your risk of developing an allergy later - especially in kids.
For asthma or hay fever, a positive IgE for dust mites or pollen might lead to environmental controls - HEPA filters, allergen-proof bedding, or immunotherapy. But again, it’s not the test alone. It’s the test + your symptoms + your lifestyle.
Final Takeaway: Knowledge Without Context Is Dangerous
Specific IgE testing is powerful - but only when used right. It’s not a magic wand. It’s not a screening tool for everyone. It’s a precision instrument for people with clear symptoms and a focused question.
Ask yourself: "Why am I doing this test?" If the answer is "just to see," stop. If the answer is "I had a reaction to eggs last week and want to know if it’s real," then yes - this test makes sense. And always, always, always bring your history to the table. The numbers are just one piece of the puzzle. Your story is the rest.







Jay Amparo January 11, 2026
I used to think IgE tests were magic. Turns out they’re more like a flashlight in a foggy room - helps a little, but you still need to know where you’re walking. My kid tested positive for peanuts at 0.8 kUA/L, ate them weekly for two years, never blinked. Now we know it’s just sensitization. Don’t panic over numbers.
Also, testing for 20 allergens? That’s like throwing darts blindfolded and calling it a diagnosis.
Lisa Cozad January 12, 2026
This is the most clear-headed breakdown of IgE testing I’ve ever read. As a nurse who’s seen parents panic over a 0.5 result, I’m so glad someone explained the context. The part about total IgE being a multiplier? Game-changer. Thanks for writing this.
Saumya Roy Chaudhuri January 13, 2026
You people don’t get it. IgE testing is the ONLY reliable method. Skin tests? Outdated. I’ve seen 17 patients with false negatives from skin prick tests because they were on Zyrtec. And don’t even get me started on those ‘I eat shrimp but test positive’ cases - that’s not a false positive, that’s your immune system being confused. You need to trust the lab, not your taste buds.
Ian Cheung January 14, 2026
So let me get this straight - you’re telling me my 12-year-old can have a 15 kUA/L peanut result and still be fine if he’s eaten peanut butter every day since kindergarten?
And if I test for 20 things I’ve never touched? I’m basically playing Russian roulette with my anxiety?
Bro. That’s wild. And also terrifying. I’m printing this out and taping it to my fridge. Maybe next time my wife wants to ‘rule out’ every food ever invented, I’ll just hand her this and say ‘read this or I’m sleeping on the couch’
Jaqueline santos bau January 16, 2026
I can’t believe people still fall for this. You’re just giving doctors an excuse to overtest. My cousin got a 20-panel test because she had a rash on her neck. Got 3 positives. Now she’s gluten-free, dairy-free, nut-free, soy-free, and still has the rash. She’s now on a $200/month ‘allergy diet’ and blames her ‘toxic body’.
It’s not science. It’s fear marketing.
Ted Conerly January 17, 2026
If you’re reading this and you’re worried about your results - breathe. The number is just one piece. Your history? That’s the whole story. I’ve had patients cry because they got a ‘positive’ for eggs and thought they’d never eat pancakes again. We looked at their history - ate them every Sunday for 30 years. No reaction. We told them to keep eating. They cried again - this time from relief.
Don’t let a number rob you of joy.
Faith Edwards January 18, 2026
The casual dismissal of component-resolved diagnostics is both scientifically negligent and intellectually lazy. The ISAC chip, while requiring expert interpretation, reduces cross-reactivity misclassification by over 60% in polysensitized individuals. To suggest that ‘standard individual testing is enough’ is to ignore the paradigm shift in allergen profiling that has been peer-reviewed since 2018.
Furthermore, the assertion that ‘your history is the key’ is not a rebuttal - it is the foundation upon which all clinical decision-making must rest. To conflate diagnostic utility with clinical utility is a fundamental error.
Kunal Majumder January 18, 2026
Man, I wish my doc in Delhi had said this 5 years ago. I got tested for 15 things because my mom was scared I’d die if I ate mango. Got 2 positives - mango and cashew. Never had a reaction to either. Still eat them. My mom still whispers ‘but the test said…’
Tests don’t lie. But people? They lie to themselves.
Aurora Memo January 20, 2026
I appreciate how this post doesn’t just list facts - it acknowledges the emotional weight behind testing. So many people feel guilty for ‘not being allergic enough’ or ashamed for ‘being too allergic.’ The truth? It’s not about being right or wrong. It’s about safety, clarity, and peace of mind.
Thank you for not turning this into a competition of who’s more allergic.
chandra tan January 20, 2026
In India, we have this thing called ‘allergy culture’ - if you sneeze once near a dog, your aunt gets you tested for 10 things. I got tested for dust mites because my cousin said ‘they live in your pillow.’ Result: 0.4 kUA/L. I sleep on the floor now.
My doctor laughed. Said ‘if you’re not wheezing, stop sleeping on the floor.’
Dwayne Dickson January 21, 2026
The notion that ‘low IgE = no risk’ is a dangerous oversimplification. In pediatric populations, IgE levels often correlate poorly with clinical reactivity in the early stages of sensitization - particularly with food allergens. The 50% probability threshold at 0.35 kUA/L for peanut is derived from cohort studies with significant selection bias.
Furthermore, the recommendation to avoid ‘panels’ is sound, but the underlying issue is systemic: primary care providers are being incentivized to order tests for revenue, not clinical indication. This is not a diagnostic problem - it’s a financial one.
anthony martinez January 23, 2026
So… if I test positive for birch pollen and my IgE for apple is 0.6, but I’ve eaten apples since I was 2… I’m just allergic to pollen and my mouth tingles?
And the test didn’t lie… I just misunderstood what it was telling me?
Wow. That’s… actually kind of beautiful.
Ritwik Bose January 24, 2026
I am pleased to note that the author has adhered to the latest guidelines from the National Institute of Allergy and Infectious Diseases (NIAID) regarding the appropriate use of specific IgE testing. Furthermore, the emphasis on component-resolved diagnostics aligns with the 2023 European Academy of Allergy and Clinical Immunology (EAACI) consensus statement.
It is imperative that patients be educated that a positive result does not equate to clinical allergy. This is not semantics - it is foundational to patient safety. 🙏
Paul Bear January 25, 2026
You say ‘don’t test for things you’ve never reacted to.’ But what if you’ve never reacted because you’ve never been exposed? What if your kid has never eaten peanuts because you’re scared? That’s not history - that’s avoidance. And avoidance increases risk.
So maybe the real question isn’t ‘why are you testing?’ - it’s ‘why are you avoiding?’
lisa Bajram January 26, 2026
I’m an ER nurse. Last week, a mom brought in her 4-year-old because he ‘tested positive’ for shellfish. He’d never eaten it. She’d been reading Reddit. He had a rash from a viral infection. She cried because she thought she’d ‘missed’ the allergy.
Don’t test for fear. Test for facts. And if you’re not sure? Ask your allergist - not your cousin’s yoga teacher who read a blog post.