Antiarrhythmic Drugs: What They Are, How They Work, and What You Need to Know
When your heart skips, races, or beats irregularly, it’s not just a flutter—it’s a signal. Antiarrhythmic drugs, medications designed to restore and maintain normal heart rhythm by targeting electrical signals in the heart. Also known as cardiac rhythm regulators, these drugs don’t cure the underlying cause, but they can stop dangerous rhythms before they lead to stroke, heart failure, or sudden death. If you’ve been told you have atrial fibrillation, ventricular tachycardia, or another type of arrhythmia, chances are you’ve been prescribed one of these. But they’re not simple pills. Each one acts differently, carries unique risks, and can interact with other meds you’re taking.
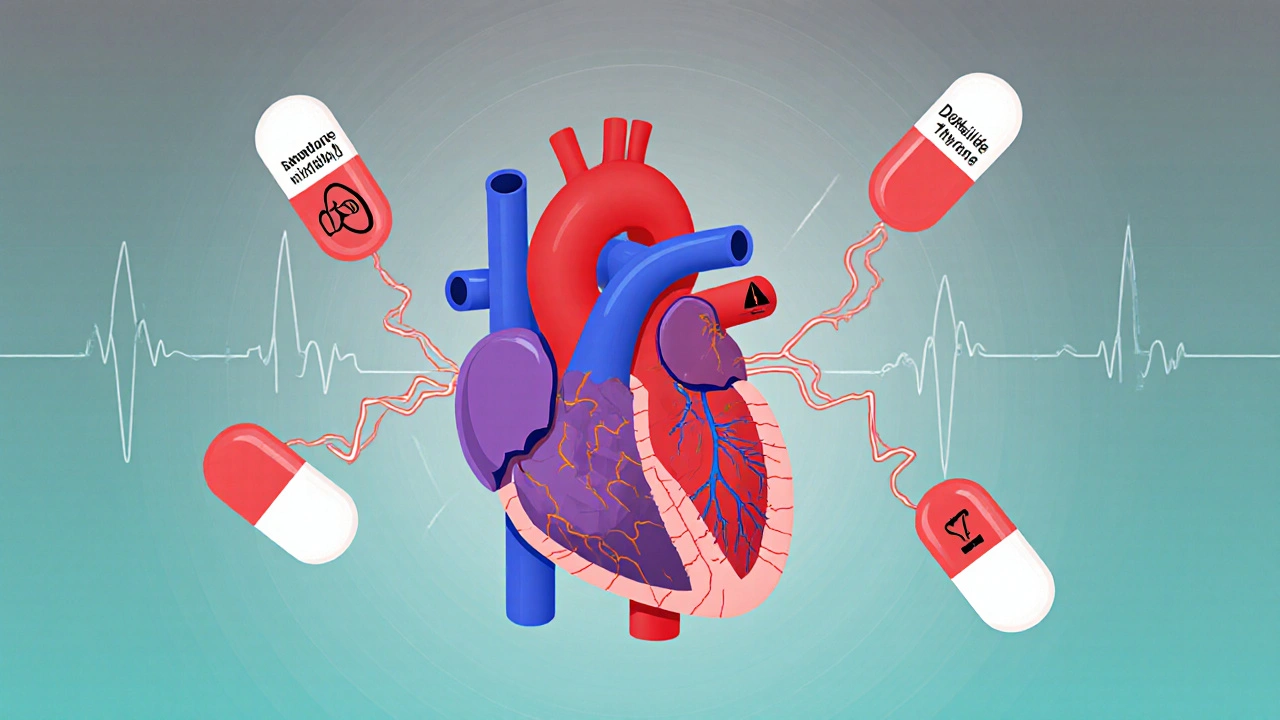
These drugs fall into four main classes, based on how they affect the heart’s electrical system. Some slow down the signals (like quinidine, a Class I antiarrhythmic that blocks sodium channels), while others lengthen the recovery time between beats (like amiodarone, a broad-spectrum Class III drug that affects potassium channels). Then there are beta-blockers like metoprolol, a Class II agent that reduces adrenaline’s effect on the heart, often used for rate control in atrial fibrillation. And calcium channel blockers like verapamil? They’re Class IV. Each has its place—but none are harmless. Amiodarone, for example, can damage your lungs or thyroid after long-term use. Quinidine can trigger a dangerous rhythm instead of fixing it. Even common drugs like antiarrhythmic drugs can become risky if you’re also taking antibiotics, antidepressants, or even grapefruit juice.
What you won’t find in most brochures is how often these drugs are used off-label, or how patients end up switching because of side effects—dizziness, fatigue, nausea, or worse. Many of the posts here dive into those real-world issues: how black box warnings apply to certain antiarrhythmics, how kidney or liver problems change dosing, and why mixing them with other meds can backfire. You’ll also see how patients manage these drugs alongside conditions like hypertension, diabetes, or even depression. This isn’t just theory. These are stories from people who’ve been on the other side of the prescription.
What you’ll find below isn’t a textbook. It’s a collection of practical, no-fluff guides written by people who’ve lived this. Whether you’re trying to understand why your doctor switched you from sotalol to dofetilide, or you’re worried about the long-term effects of amiodarone, or you just want to know what to ask when your heart starts acting up again—this is where you start. No jargon. No marketing. Just what you need to know to stay safe and informed.
Compare Cordarone (Amiodarone) with Alternatives: What Works Best for Arrhythmias
Cordarone (Amiodarone) is a powerful but risky heart rhythm drug. Learn how it compares to safer alternatives like sotalol, dofetilide, and dronedarone - and when each option makes sense.