Proton Pump Inhibitors: What They Are, How They Work, and What You Need to Know
When your stomach makes too much acid—causing heartburn, ulcers, or damage to your esophagus—proton pump inhibitors, a class of drugs that block the final step of acid production in the stomach lining. Also known as PPIs, they’re among the most prescribed medications in the world for acid-related conditions. Unlike antacids that just coat the acid, PPIs stop it at the source. They work by targeting the proton pumps in stomach cells—the tiny machines that pump acid into your stomach. Turn those off, and acid production drops dramatically.
Common PPIs include omeprazole, esomeprazole, lansoprazole, and pantoprazole. You’ll find them over the counter or by prescription, depending on strength and use. They’re used for GERD, a chronic condition where stomach acid flows back into the esophagus, peptic ulcers, Zollinger-Ellison syndrome, and sometimes to protect the stomach when taking NSAIDs. But they’re not harmless. Long-term use has been linked to kidney issues, bone fractures, and nutrient deficiencies like magnesium and B12. The FDA has issued warnings about these risks, especially when used for years without medical supervision.
Many people take PPIs for months or even years without realizing they might not need them. Some use them for occasional heartburn, but that’s what antacids or H2 blockers like famotidine are for. PPIs take 1–4 days to reach full effect, so they’re not ideal for quick relief. And stopping them suddenly can cause rebound acid hypersecretion—your stomach overcompensates and makes even more acid than before. That’s why tapering off under a doctor’s guidance matters.
There are alternatives. Lifestyle changes like avoiding spicy food, eating smaller meals, and not lying down after eating can reduce acid reflux. H2 blockers offer a shorter-term option with fewer long-term risks. And for some, the real issue isn’t too much acid—it’s a weak lower esophageal sphincter or a hiatal hernia. In those cases, PPIs mask the symptom, not the cause.
What you’ll find below is a collection of real, practical articles that dig into the risks, alternatives, and hidden connections of acid-reducing drugs. You’ll see how PPIs interact with other medications, why they’re linked to kidney problems, and what to do if you’ve been taking them longer than you should. These aren’t theory pieces—they’re based on clinical findings, patient experiences, and safety alerts from trusted sources like the FDA. Whether you’re considering stopping your PPI, managing side effects, or just trying to understand why your doctor prescribed it, this list gives you the clear, no-fluff facts you need.
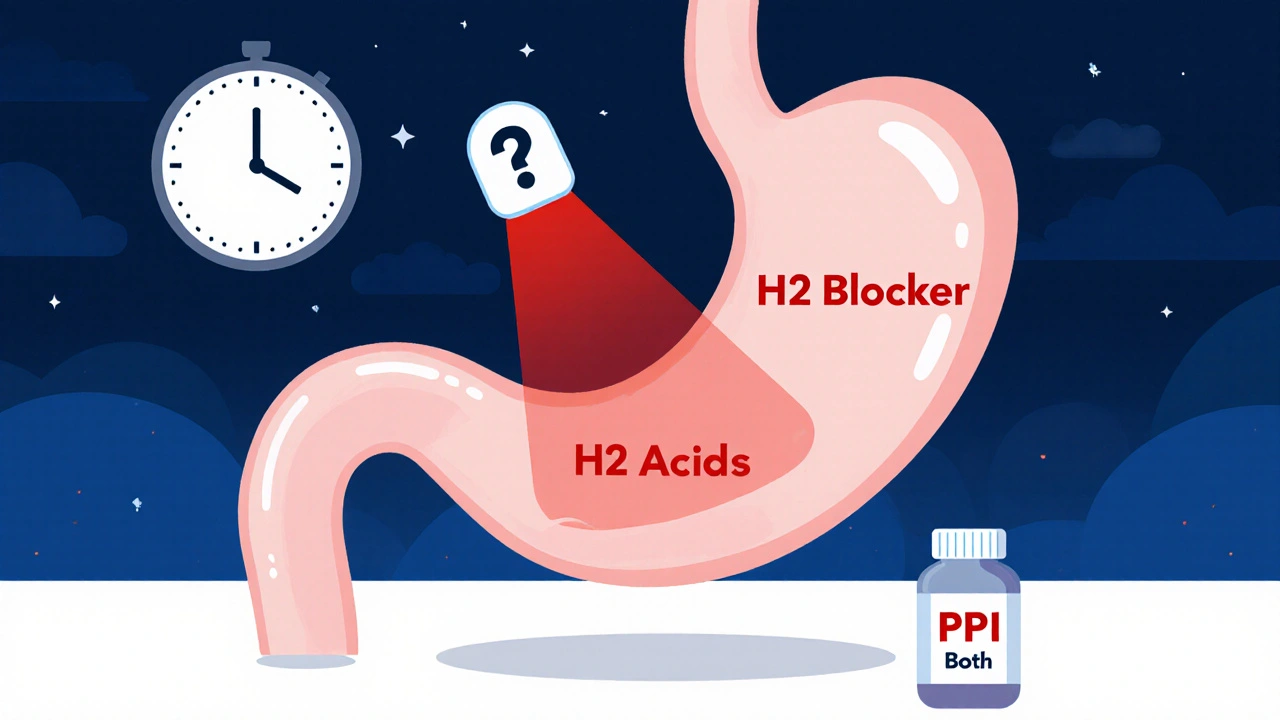
H2 Blockers and PPIs: When Combining Acid Reducers Does More Harm Than Good
Combining H2 blockers and PPIs is common but often unnecessary. Learn why this practice increases risks without improving outcomes-and what to do instead.