If you’re struggling to pay for prescriptions, you’re not alone. In 2025, 28% of Medicare beneficiaries still say they can’t afford their medications. But help exists-through state-run programs that can slash your monthly drug costs by hundreds of dollars. These aren’t myths or distant possibilities. They’re real, active programs in every state, with different rules, coverage, and income limits. Knowing which one you qualify for could mean the difference between taking your insulin or skipping doses.
What Exactly Are State Pharmaceutical Assistance Programs (SPAPs)?
State Pharmaceutical Assistance Programs, or SPAPs, are government-funded programs that help people pay for prescription drugs. They’re run by individual states, not the federal government, so each one works differently. Some cover only seniors. Others include people with disabilities or low incomes. A few even help people who have Medicare Part D but still can’t afford their copays.
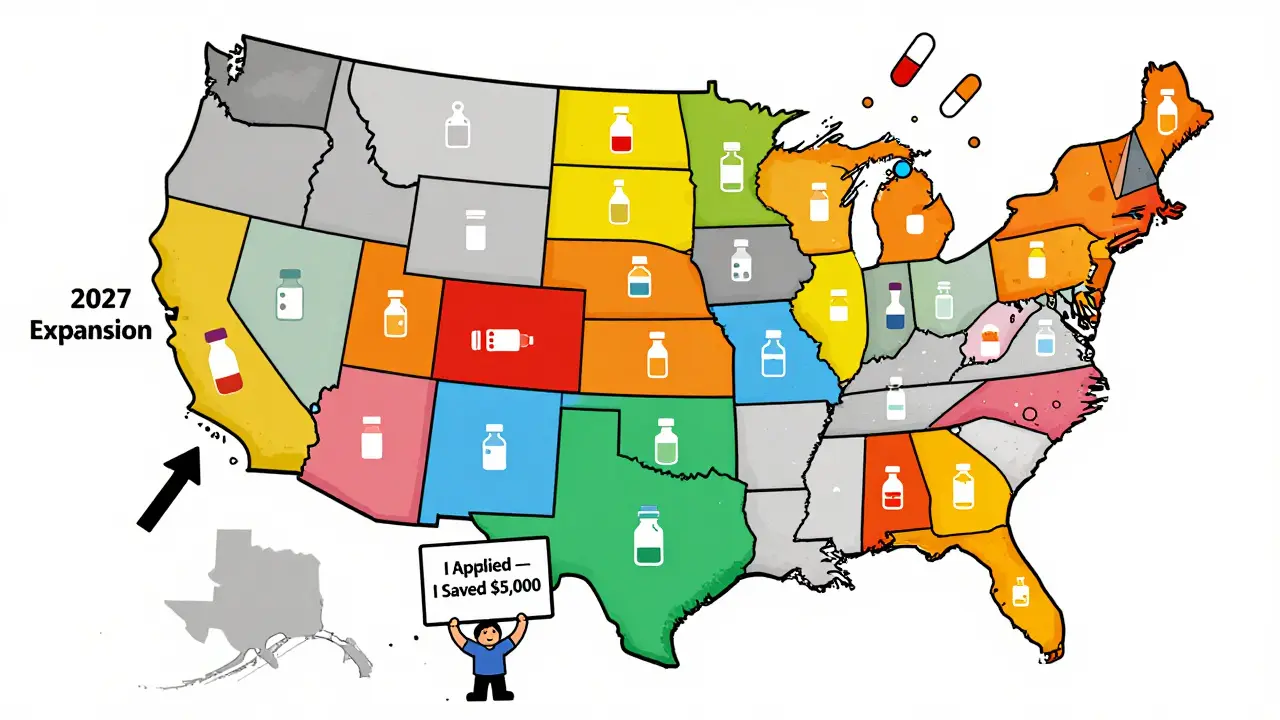
Thirty-two states have some kind of SPAP in 2025. The budgets range from $15 million in Wyoming to $215 million in Pennsylvania. These programs don’t replace Medicare-they work alongside it. In states like New Jersey and Pennsylvania, SPAPs pay your Part D premiums, cover drugs Medicare doesn’t, or lower your copays to just $5 or $7 per prescription.
Unlike federal programs, SPAPs can be more flexible. For example, California’s Medi-Cal Rx program includes 127 specialty drugs that aren’t on standard Medicare Part D formularies. That’s huge for people with conditions like multiple sclerosis or rheumatoid arthritis who rely on expensive biologics.
Medicare Extra Help: The Federal Safety Net
If you’re on Medicare and have limited income, you might qualify for Extra Help-a federal program run by Social Security. It’s not state-specific, so it’s the same no matter where you live. In 2025, the income limits are $23,475 for individuals and $31,725 for married couples. Resource limits are $17,600 and $35,130, respectively. These numbers went up 3.9% from 2024.
What does Extra Help actually do? If you qualify, you pay $0 for your Medicare Part D premium and deductible. For generics, your copay is $4.90. For brand-name drugs, it’s $12.15. That’s lower than most state programs. You also get automatic enrollment in a drug plan if you don’t have one.
But here’s the catch: Extra Help has strict rules. If your savings account has $18,000, you’re denied-even if you live in San Francisco and rent an apartment for $2,800 a month. Critics say the resource limits don’t match real-life costs. A 2024 KFF analysis found that many people in high-cost states are turned away simply because they own a car or have a small savings account.
How New Jersey’s PAAD Program Works
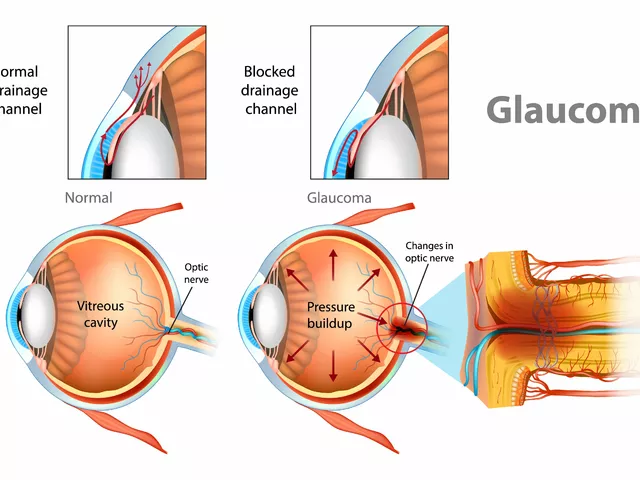
New Jersey’s Pharmaceutical Assistance to the Aged and Disabled (PAAD) is one of the oldest and most generous SPAPs. Started in 1967, it’s been a lifeline for over 200,000 residents. In 2025, PAAD covers all prescription drugs, insulin, and syringes for injectable MS treatments.
Eligibility is based on age (65+) or disability, plus income under $33,500 for individuals or $40,000 for couples. You must be enrolled in Medicare Part D, but PAAD pays your premium if it’s $34.70 or less per month. Your copays? $5 for generics, $7 for brand-name drugs. That’s far below the national average of $15-$25.
One user on Reddit wrote: “After losing my employer coverage at 65, PAAD saved me over $400 monthly on my diabetes meds.” But there’s a downside. If your doctor prescribes a drug not on PAAD’s formulary, you have to appeal. The process takes 6-8 weeks. During that time, you go without.

Pennsylvania’s PACE: More Than Just Copays
Pennsylvania’s Pharmaceutical Assistance Contract for the Elderly (PACE) goes further than most SPAPs. It doesn’t just cover copays-it pays for drugs Medicare won’t. If your Part D plan doesn’t cover a medication, PACE will. That’s rare.
In 2025, income limits are $27,470 for individuals and $36,900 for couples. You must apply for Extra Help first. Only after that does PACE kick in to cover the rest. This two-step process takes an average of 120 days to complete. Many people give up before it’s done.
But for those who make it through, the savings are massive. One retiree in Pittsburgh said, “I take six medications. Without PACE, I’d be paying $900 a month. Now it’s $40.”
Why State Programs Vary So Much
There’s no national standard for drug assistance. Why? Because each state sets its own rules based on budget, population needs, and political will.
Some states use Average Wholesale Price (AWP) minus 20% to pay pharmacies. Others use Wholesale Acquisition Cost (WAC) plus a $5 dispensing fee. Seven states use a mix. These differences affect how much pharmacies get paid-and whether they’ll even fill your prescription.
Also, formularies change. In 2024, 18 states cut coverage or added prior authorization rules to save money. That means a drug you got last year might be denied this year. You’ll need to reapply or appeal.
The result? A patchwork system. If you move from New Jersey to Florida, your PAAD benefits vanish. You’ll have to start over with Florida’s program-if it even exists. A 2024 Medicare Rights Center study found that 63% of people who moved between states had a gap in coverage. Some went weeks without meds.
How to Apply: The Real Process
Applying for Extra Help means filling out the SSA-1020 form. You’ll need your tax return, bank statements, proof of residence, and a list of your medications. Processing takes about 90 days. During that time, you pay full price. One person on the Medicare Rights Center forum paid $872 out of pocket for a heart medication while waiting.
State programs vary. New Jersey’s PAAD takes 30 days on average. But if you’re missing documents, it can stretch to 90. Most require annual re-certification. You’ll get a notice in the mail. If you ignore it, your benefits stop.
There’s help available. Every state has a State Health Insurance Assistance Program (SHIP). They offer free, one-on-one counseling. There are 14,000 certified counselors nationwide. They’ll walk you through forms, explain your options, and even call your pharmacy to check formulary status.
Who Gets Left Behind?
Despite all this, only 42% of eligible people actually enroll. Why? Complexity. Confusion. Fear.
Dr. Aaron Kesselheim from Harvard says, “The system is designed for people who can spend eight hours filling out forms and chasing paperwork. That’s not most seniors.”
People with cognitive decline, limited English skills, or no internet access are especially vulnerable. A 2024 KFF survey found that 28% of Medicare beneficiaries still struggle to afford drugs. That number jumps to 41% for those not enrolled in any assistance program.
Even with the Inflation Reduction Act’s new $2,000 annual out-of-pocket cap for Part D in 2025, many won’t know they qualify. The cap doesn’t apply unless you’re enrolled in Extra Help or a state program. If you don’t apply, you pay the full cost.
What’s Changing in 2025 and Beyond
Big changes are coming. Starting in 2025, people on Extra Help or Medicaid can switch their Medicare drug plan once a month-not just once a year. That’s huge for people whose meds change often.
Also, 12 more states are expected to launch or expand SPAPs by 2027. California, Texas, and Florida are leading the charge. They’re focusing on specialty drugs, which are rising 12.3% per year-faster than state budgets can keep up.
But sustainability is a problem. Seven states are projected to face funding shortfalls by 2026. If you’re counting on your state’s program to last, check its budget history. Some have cut coverage every year since 2020.
What You Should Do Right Now
Don’t wait. If you’re on Medicare and take prescriptions, here’s your action plan:
- Go to Medicare.gov and use the Extra Help application tool. It takes 10 minutes.
- Call your State Health Insurance Assistance Program (SHIP). Find your local office at shiptacenter.org. They’ll help you apply for state programs too.
- Write down every medication you take. Check if they’re on your state’s formulary. If not, ask about appeals.
- Don’t assume you’re not eligible. Many people think they make too much money-but the limits are higher than you think.
- Apply before March 2025. Processing delays are common. You don’t want to go without meds in the summer.
People who qualify save $4,000 to $5,000 a year on prescriptions. That’s not a small amount. It’s rent. It’s groceries. It’s keeping your health from falling apart.
These programs exist to help you. But they won’t find you. You have to find them.
Do I qualify for Medicare Extra Help if I’m on Medicaid?
Yes. If you’re enrolled in Medicaid, you automatically qualify for Extra Help. You don’t need to apply separately. Social Security will enroll you automatically. You’ll get the lowest possible copays: $4.90 for generics and $12.15 for brand-name drugs.
Can I get help from both my state program and Medicare Extra Help?
Yes, and that’s often the best strategy. In states like Pennsylvania and New Jersey, you apply for Extra Help first. Then your state program (PACE or PAAD) covers what’s left-like your Part D premium or drugs Medicare doesn’t cover. This stacking of benefits can reduce your annual drug costs by over $5,000.
What if my state doesn’t have a pharmaceutical assistance program?
Twelve states don’t have SPAPs, but you can still get help through Medicare Extra Help. Even without state support, Extra Help cuts your copays to $4.90 and $12.15. You can also check with local charities, drug manufacturers’ patient assistance programs, or nonprofit pharmacies like NeedyMeds.org for additional discounts.
Why do some medications get denied by state programs?
Each state has a formulary-a list of approved drugs. If your drug isn’t on it, the program won’t pay. This happens often with specialty drugs or newer medications. You can appeal, but it takes 6-8 weeks. During that time, you may need to pay full price or ask your doctor for a substitute.
How often do I need to reapply for state assistance?
Most state programs require annual re-certification. You’ll get a form in the mail. You’ll need to submit updated income documents-usually your tax return or Social Security statement. If you don’t respond, your benefits stop. Set a calendar reminder for the same month each year.



James Hilton December 28, 2025
So let me get this straight-we’re telling seniors to jump through 17 hoops just to afford insulin? And we wonder why people die in garages.
Mimi Bos December 29, 2025
i just applied for paad last week and they lost my form… twice. now im waiting for a call back. why does this feel like playing telephone with the government?
sonam gupta December 29, 2025
in india we dont have such programs but we buy generic meds from bangladesh for 10% price
Vu L December 31, 2025
Wait so you’re telling me the government gives you money to buy drugs but only if you’re poor enough to qualify but not poor enough to need it? Classic.
Celia McTighe January 2, 2026
This is so important. I just helped my neighbor apply for Extra Help-she cried when she found out she’d save $300/month. We need more people to know this exists. 💙
Sydney Lee January 2, 2026
It's not merely a bureaucratic failure-it's a moral collapse. The very architecture of American healthcare is predicated on the assumption that suffering is a necessary tax for citizenship. And yet, we call this freedom.
oluwarotimi w alaka January 4, 2026
they dont want you to know this. big pharma owns every state house. they let you suffer so you'll keep buying their overpriced pills. its all a scam. i saw it on a video. the government is in bed with the drug lords. dont trust any of this.
Payton Daily January 4, 2026
Think about it. Why does it take 120 days to get help when your kidneys are failing? Because the system was built by people who never had to choose between insulin and rent. We're not broken. We're designed this way. The real question is-why are we surprised?
Kelsey Youmans January 6, 2026
Thank you for compiling this comprehensive and meticulously researched overview. The structural inequities illuminated here demand urgent policy intervention. I have shared this with my state’s legislative aide.
Debra Cagwin January 6, 2026
If you’re reading this and feeling overwhelmed-start with one step. Just one. Call SHIP. They won’t judge you. They’ve seen it all. You don’t have to fix everything today. Just get started. You’re not alone.
Hakim Bachiri January 8, 2026
Okay, but why is it that every time someone tries to fix this, the politicians just add another form?!!??!!?? And then they wonder why people give up?!!??!!??
Ryan Touhill January 9, 2026
There's a reason these programs are so complex. It's not incompetence-it's intentional exclusion. The wealthy want to believe the poor are lazy, not systemic. If it were easy, everyone would qualify. And then they'd have to pay taxes. That's the real fear.
Julius Hader January 10, 2026
My aunt got PAAD last year. She’s been taking her meds since. No more skipping doses. No more crying at the pharmacy. Just… peace. 🙏