Understanding Atrophic Gastroenteritis and Gastroesophageal Reflux Disease
As a blogger who often discusses various gastrointestinal issues, I have come to realize that many people are not familiar with the connection between atrophic gastroenteritis and gastroesophageal reflux disease (GERD). In this article, I will provide a comprehensive overview of these two conditions and discuss their interrelationship.
A Brief Overview of Atrophic Gastroenteritis
Atrophic gastroenteritis is a chronic inflammatory condition that affects the lining of the stomach. It is characterized by a gradual loss of gastric glands, leading to a reduction in the production of gastric acid and digestive enzymes. This, in turn, impairs the stomach's ability to break down and absorb nutrients from food, leading to various nutritional deficiencies and gastrointestinal symptoms such as abdominal pain, bloating, and diarrhea.
The exact cause of atrophic gastroenteritis is not yet fully understood, but it is believed to be a result of a combination of genetic and environmental factors. Some common risk factors include advanced age, a history of Helicobacter pylori infection, and autoimmune disorders such as pernicious anemia.
What is Gastroesophageal Reflux Disease (GERD)?
Gastroesophageal reflux disease, or GERD, is a common digestive disorder that occurs when stomach acid or bile flows back into the esophagus, causing irritation and inflammation. This backward flow, or reflux, can lead to damage of the esophageal lining and produce symptoms such as heartburn, chest pain, difficulty swallowing, and regurgitation of food or sour liquid.
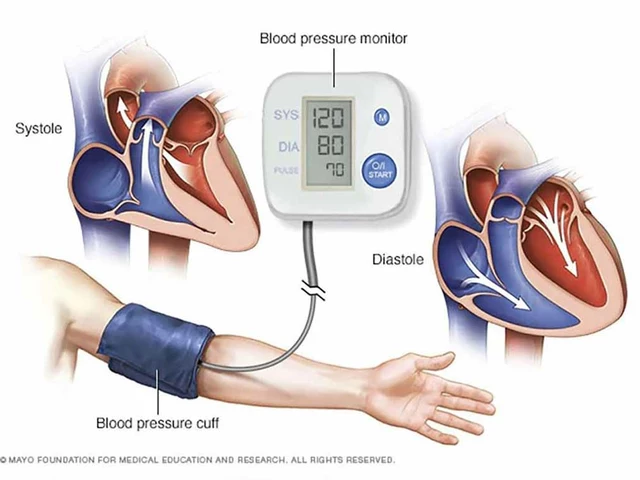
The primary cause of GERD is a weakened lower esophageal sphincter (LES), which is a ring of muscle that acts as a valve between the esophagus and stomach. When functioning properly, the LES opens to allow food to enter the stomach and then closes to prevent reflux. However, in individuals with GERD, the LES does not close properly, allowing acid to flow back into the esophagus.
Common Risk Factors for GERD
There are several factors that can increase the risk of developing GERD, including obesity, pregnancy, smoking, and the consumption of certain foods and beverages (such as fried or fatty foods, chocolate, alcohol, and caffeine). Additionally, certain medications, such as calcium channel blockers, antihistamines, and pain relievers, can also contribute to the weakening of the LES and the development of GERD.
It is important to identify and address these risk factors in order to prevent or manage GERD effectively. Lifestyle modifications, such as weight loss, smoking cessation, and dietary changes, can often help alleviate GERD symptoms and reduce the need for medications.
How Atrophic Gastroenteritis and GERD are Connected
Atrophic gastroenteritis and GERD may appear to be unrelated conditions at first glance, but they share a common underlying problem: the disruption of normal gastric function. In atrophic gastroenteritis, the reduction in gastric acid production can lead to a condition known as hypochlorhydria, which is characterized by abnormally low levels of stomach acid. This can have several consequences, one of which is an increased risk of developing GERD.
Low stomach acid can impair the LES's ability to close properly, allowing acid to reflux into the esophagus. Furthermore, the reduced acidity in the stomach can alter the balance of gastrointestinal bacteria, leading to an overgrowth of harmful bacteria that can further exacerbate GERD symptoms.
Diagnosing GERD and Atrophic Gastroenteritis
If you suspect that you may have either atrophic gastroenteritis or GERD, it is important to consult with a healthcare professional to obtain an accurate diagnosis. A thorough evaluation will typically involve a review of your medical history, a physical examination, and various diagnostic tests, such as endoscopy, biopsy, and pH monitoring.
Once a diagnosis has been made, your healthcare provider will work with you to develop an appropriate treatment plan tailored to your specific needs and circumstances.
Treatment Options for GERD and Atrophic Gastroenteritis
The treatment of GERD and atrophic gastroenteritis typically involves a combination of lifestyle modifications, medications, and, in some cases, surgical intervention. For GERD, lifestyle modifications may include weight loss, dietary changes, and elevating the head of the bed during sleep. Medications commonly used to treat GERD include antacids, H2 blockers, and proton pump inhibitors (PPIs).
In the case of atrophic gastroenteritis, treatment may involve addressing the underlying cause (such as eradicating H. pylori infection) and supplementing with vitamins and minerals to correct any nutritional deficiencies. If GERD is present in conjunction with atrophic gastroenteritis, it may be necessary to use medications to reduce acid reflux and protect the esophageal lining.
Living with GERD and Atrophic Gastroenteritis
Though both GERD and atrophic gastroenteritis can be challenging to manage, it is possible to live a healthy and fulfilling life with these conditions. By working closely with your healthcare provider, making necessary lifestyle changes, and adhering to your prescribed treatment plan, you can effectively manage your symptoms and prevent complications.
Remember, it is important to be proactive in your care and to communicate openly with your healthcare team about any concerns or questions you may have. With the right support and resources, you can successfully navigate life with GERD and atrophic gastroenteritis.




beth shell June 2, 2023
We often overlook how the silent erosion of gastric glands reshapes the very dialogue between our stomach and esophagus, a subtle shift that can echo as reflux.
khushali kothari June 3, 2023
The etiopathogenesis of atrophic gastroenteritis is frequently ascribed to a confluence of immunological derangements and microbial perturbations.
Chronic Helicobacter pylori colonization initiates a cascade of cytokine-mediated glandular apoptosis, culminating in mucosal atrophy.
Concurrently, autoimmune pernicious anemia precipitates intrinsic factor deficiency, exacerbating parietal cell loss.
The resultant hypochlorhydria engenders a milieu conducive to bacterial overgrowth and altered gastric pH homeostasis.
This dysregulated environment potentiates the relaxation of the lower esophageal sphincter, thereby facilitating gastroesophageal reflux.
Moreover, the diminution of acidic luminal content impairs the feedback inhibition of gastrin secretion, provoking hypergastrinemia.
Elevated gastrin levels have been documented to modulate transient lower esophageal sphincter relaxations through vagal pathways.
Endoscopic assessment frequently reveals a flattened gastric rugae pattern coupled with erythematous esophageal mucosa.
pH-metric studies typically demonstrate increased reflux episodes correlated with attenuated nocturnal acid peaks.
Therapeutic algorithms advocate for eradication of H. pylori, supplementation of vitamin B12, and judicious use of proton pump inhibitors.
However, indiscriminate proton pump inhibitor administration may further attenuate gastric acidity, paradoxically sustaining reflux pathophysiology.
Probiotic adjuncts have emerged as a viable strategy to restore microbiota equilibrium and mitigate symptomatology.
Nutritional counseling emphasizing low-fat, non-spicy diets can attenuate esophageal exposure to irritants.
Longitudinal cohort analyses indicate that early intervention in atrophic gastritis may curtail the progression to reflux-associated complications such as Barrett’s esophagus.
Consequently, an integrative approach encompassing antimicrobial, endocrine, and lifestyle modalities is paramount for optimal patient outcomes.
Brandon Smith June 3, 2023
It's astonishing how many people eat junk and blame their reflux on mysterious gut conditions instead of accepting personal responsibility for their dietary choices.
darwin ambil June 3, 2023
🤔 lol, you’re right, but not everyone knows the science behind LES dysfunction – a quick read can save a lot of heartburn! 😅
Kelvin Van der Maelen June 3, 2023
This whole thing is a health nightmare straight out of a horror movie.
Joy Arnaiz June 3, 2023
One must consider the possibility that pharmaceutical conglomerates are suppressing alternative treatments for atrophic gastroenteritis to maintain profit margins, a tactic evident in the selective funding of clinical trials.