Insulin Biosimilars: What They Are, How They Compare, and What You Need to Know
When you need insulin to manage diabetes, you’re not just buying a drug—you’re buying stability, safety, and daily control. Insulin biosimilars, highly similar versions of brand-name insulin products approved by regulatory agencies after the original patent expires. Also known as follow-on insulins, they work the same way in your body but often cost significantly less. This isn’t theoretical. In the U.S. and Europe, insulin biosimilars like insulin glargine-ynfg (Semglee) and insulin lispro-aabc (Admelog) are already replacing older, pricier versions in clinics and pharmacies. They’re not generics—they’re complex biological products made from living cells, which is why they’re called biosimilars, not generics.
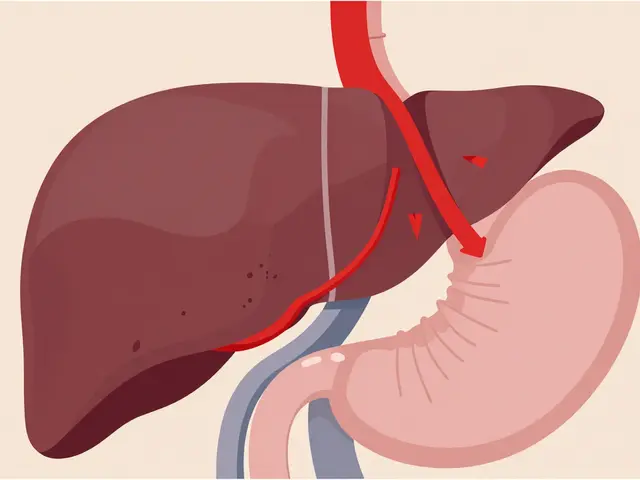
Insulin biosimilars relate directly to other diabetes treatments you might see in our posts, like GLP-1 agonists, medications like tirzepatide and semaglutide that help control blood sugar and promote weight loss. While GLP-1 drugs are newer and often used alongside insulin, biosimilars give you more options if you’re already on insulin. They also connect to medication absorption, how your body takes in drugs like insulin or fiber supplements. If you’re switching from a brand-name insulin to a biosimilar, timing and injection technique still matter. Your body doesn’t care about the brand name—it cares about the dose, the timing, and whether your blood sugar stays in range.
Cost is the biggest driver behind the shift to biosimilars. A vial of brand-name insulin can cost over $250. A biosimilar version? Often under $100. That’s life-changing for people on fixed incomes. But it’s not just about price. Safety is just as important. Biosimilars go through strict testing to prove they match the original in purity, potency, and clinical effect. The FDA doesn’t approve them lightly. Still, some patients worry about switching. That’s normal. If you’ve been stable on one insulin for years, changing—even to something identical—can feel risky. But thousands of people have switched successfully. The key? Talk to your doctor. Don’t switch on your own. Monitor your levels closely for the first few weeks. Keep a log. If your blood sugar starts to swing, don’t assume it’s the biosimilar—it could be stress, diet, or illness.
Our collection of posts dives into the real-world side of medication use. You’ll find guides on how insulin interacts with other drugs, how to avoid dangerous combinations, and how to manage side effects like low blood sugar or weight gain. You’ll also see how other medications—like opioids, acid reducers, or antibiotics—can interfere with your diabetes care. We don’t just list facts. We show you what actually works when you’re juggling multiple prescriptions, tight budgets, and busy schedules.
Insulin Biosimilars: What You Need to Know About Cost, Safety, and Market Options
Insulin biosimilars offer the same effectiveness as branded insulins at 30% lower cost. Learn how they work, which ones are available, why adoption is slow, and how to switch safely.