When your liver is damaged, blood doesn’t flow through it the way it should. That’s when portal hypertension kicks in - a silent, dangerous rise in pressure inside the main vein that carries blood from your gut to your liver. It’s not a disease on its own. It’s a consequence. And if left unchecked, it can lead to bleeding varices, fluid buildup in your belly, and even brain fog or kidney failure. For people with cirrhosis, this isn’t theoretical. It’s daily reality.
What Exactly Is Portal Hypertension?
Portal hypertension means the pressure in the portal vein - the big blood vessel that brings nutrient-rich blood from your intestines to your liver - has climbed above 10 mmHg. Normal pressure? 5 to 10 mmHg. Once it hits 10 or higher, you’ve crossed into clinically significant territory. The gold standard for measuring this? The hepatic venous pressure gradient, or HVPG. If your HVPG is above 5 mmHg, you’ve got portal hypertension. Above 10 mmHg? You’re at high risk for serious complications.Over 90% of cases come from cirrhosis. That’s scarring. That’s your liver turning stiff, like a dried-out sponge. Blood can’t flow through easily. The rest? Non-cirrhotic causes - things like blood clots in the portal vein, rare liver diseases, or even certain infections. But cirrhosis? That’s the big one. And with non-alcoholic fatty liver disease (NAFLD) rising fast, we’re seeing more cases than ever before.
Why Varices Are a Medical Emergency
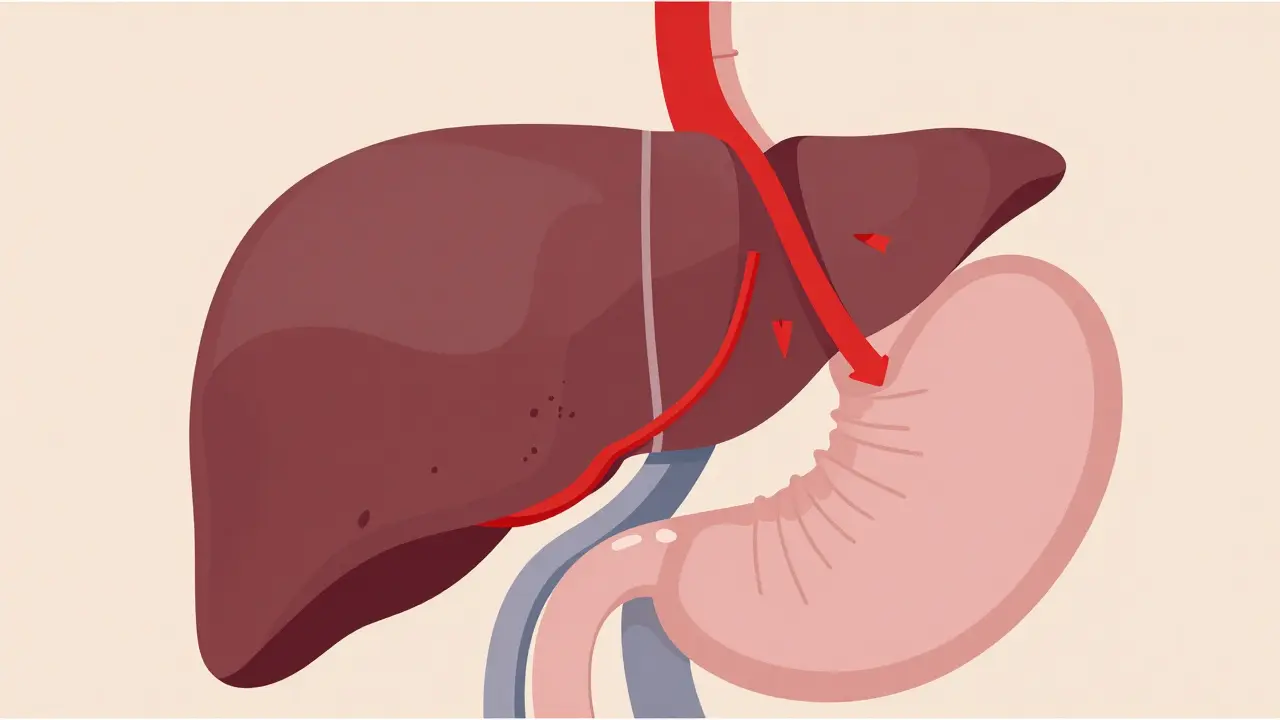
When blood can’t flow through the liver, it finds other paths. Those paths are weak veins - especially in your esophagus and stomach. These are varices. Think of them like overinflated, thin-walled balloons filled with blood under high pressure. They’re not supposed to be there. And when they rupture? It’s catastrophic.Half of all people with cirrhosis develop varices within 10 years. And each year, 5 to 15% of those with medium-to-large varices will bleed. That’s not a small number. That’s life-or-death territory. Vomiting blood, passing black tar-like stools - these aren’t just symptoms. They’re warning signs screaming for immediate help.
The standard response? Emergency endoscopy within 12 hours. While you’re being rushed to the hospital, doctors will start vasoactive drugs like terlipressin or octreotide to slow blood flow to the varices. Antibiotics - usually ceftriaxone - are given right away. Why? Because infection risk spikes after bleeding, and it kills.
Once the bleeding is under control, band ligation is the go-to. A tiny rubber band is placed around the varix during endoscopy. It cuts off blood flow. The varix shrivels up and falls off. It’s not glamorous, but it works. After one session, rebleeding drops from 60% to under 30%. Repeat sessions are often needed. And long-term? Non-selective beta-blockers like propranolol are prescribed. They lower heart rate and reduce pressure in the portal system. Take them daily. Skip them? Your risk of another bleed jumps back up.
Ascites: When Your Belly Swells for No Apparent Reason
Sixty percent of people with cirrhosis develop ascites - fluid pooling in the abdomen - within a decade. It’s not just uncomfortable. It’s debilitating. You can’t lie flat. You can’t walk far. Your clothes don’t fit. Your breathing gets shallow. And if you’ve ever had a paracentesis - where a needle drains the fluid - you know the relief. But also the burden.First-line treatment? Salt restriction. Less than 2,000 mg a day. That’s harder than it sounds. Processed food, restaurant meals, even bread - they’re all loaded with sodium. Then come the diuretics. Spironolactone (100 mg/day) and furosemide (40 mg/day) are the standard combo. They help your kidneys flush out extra fluid. For most people, this works. Up to 95% of cases respond.
But if your belly is rock hard and you’re struggling to breathe? You need a large-volume paracentesis. Up to 6 liters of fluid pulled out in one session. That’s a lot. And when you remove that much fluid, your body goes into shock unless you replace it with albumin - about 6 to 8 grams for every liter removed. It’s expensive. It’s invasive. But it saves lives.
Some people develop refractory ascites - fluid that won’t respond to diuretics or keeps coming back. That’s when TIPS comes in. Transjugular intrahepatic portosystemic shunt. Sounds complicated? It is. A stent is placed inside the liver to create a shortcut between the high-pressure portal vein and the low-pressure hepatic vein. It lowers pressure. It reduces fluid. Success rate? 90%. But there’s a catch. About 20 to 30% of patients develop hepatic encephalopathy after TIPS - confusion, memory loss, even coma. It’s a trade-off.
The Hidden Complications Nobody Talks About
Portal hypertension doesn’t just affect your belly or your esophagus. It messes with your brain, your kidneys, your whole system.Hepatic encephalopathy - brain dysfunction from liver failure - hits 30 to 45% of cirrhotic patients. Toxins like ammonia build up because your liver can’t filter them. You might forget names. You might slur your words. You might sleep all day. It’s not dementia. It’s liver failure showing up in your mind. Rifaximin and lactulose are the go-to treatments. They trap toxins in your gut so your body can flush them out.
Hepatorenal syndrome is even scarier. Your kidneys start failing - not because they’re damaged, but because your body redirects blood away from them to protect your heart and brain. It happens in 18% of hospitalized patients with ascites. Survival without a transplant? Less than 50% at six months. It’s a death sentence unless you get a new liver.
And then there’s the emotional toll. Patients on forums describe living in constant fear - of vomiting blood, of waking up swollen, of forgetting who their children are. One nurse quit her job because she couldn’t stand for more than 20 minutes. Another said the terror of bleeding was worse than any pain he’d ever felt.
What’s New in 2026? The Future Is Here
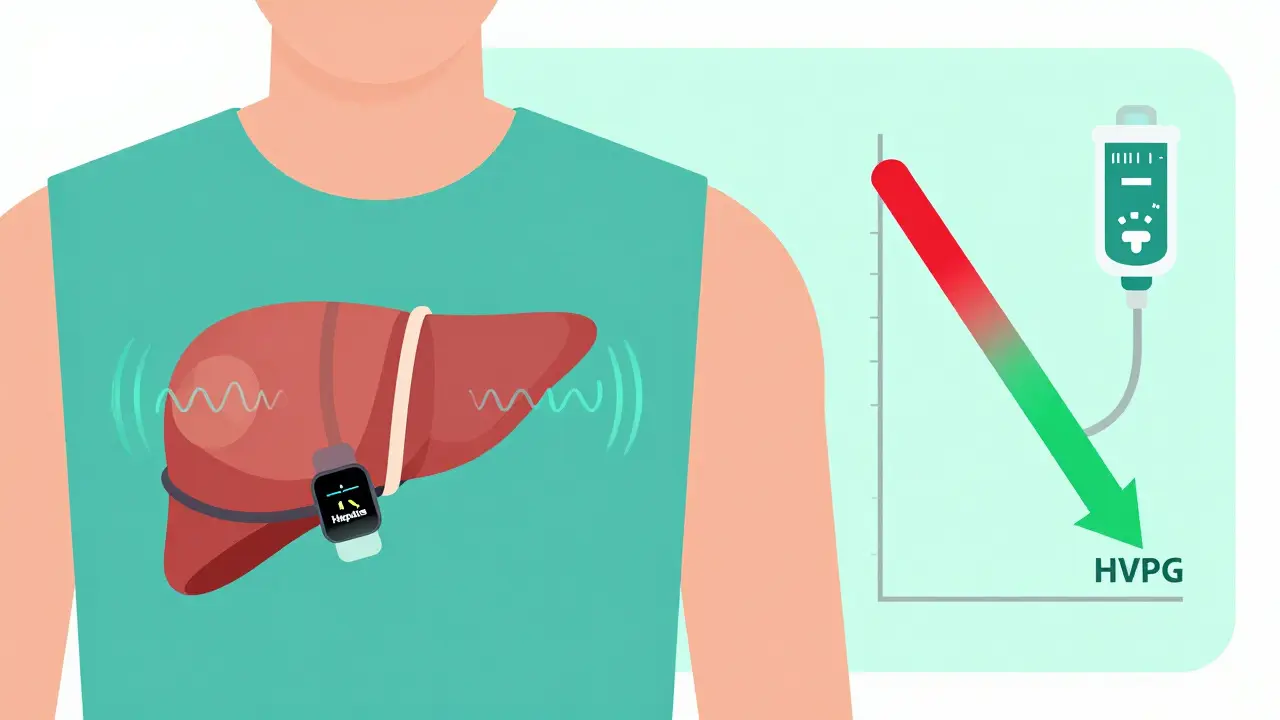
We’re moving beyond just managing symptoms. New tools are changing the game.In 2023, the FDA approved the Hepatica SmartBand - a wearable that estimates portal pressure using bioimpedance. No needles. No catheters. Just a strap around your chest. It’s 82% accurate compared to HVPG. That’s huge. It could make monitoring routine instead of rare.
Non-invasive tests like spleen stiffness measurement via elastography are hitting 85% accuracy in predicting high-risk portal hypertension. That means we might soon skip invasive HVPG tests for many patients.
And drugs? Simtuzumab, a monoclonal antibody targeting liver scarring, got breakthrough designation from the FDA in late 2023. Phase 3 trials showed a 35% drop in HVPG. That’s not just symptom control. That’s disease modification.
Artificial intelligence is stepping in too. Mayo Clinic’s AI model predicts variceal bleeding with 92% accuracy - better than any doctor relying on symptoms alone. It analyzes scans, lab results, and even voice patterns to spot risk before it’s obvious.
What You Need to Know Right Now
If you have cirrhosis or are at risk:- Get your HVPG checked if your doctor hasn’t already. It’s the only way to know your true risk.
- Take your beta-blockers daily - even if you feel fine. They prevent bleeding.
- Watch your salt. No more canned soups, chips, or takeout. Cook at home.
- Know the signs of bleeding: black stools, vomiting blood, dizziness, rapid heartbeat.
- Know the signs of encephalopathy: confusion, forgetfulness, slurred speech, tremors.
- Ask about non-invasive monitoring like elastography if HVPG isn’t available.
Portal hypertension isn’t curable - yet. But it’s manageable. With the right care, many people live years with good quality of life. The key? Early detection. Strict adherence. And never ignoring the warning signs.
When to Call 911
If you have portal hypertension and experience any of these, go to the ER immediately:- Vomiting bright red blood or coffee-ground material
- Black, tarry, or bloody stools
- Sudden, severe abdominal pain
- Confusion, drowsiness, or inability to stay awake
- Shortness of breath with rapid swelling of the abdomen
These aren’t waiting-room symptoms. They’re emergency signals. Don’t call your doctor. Don’t wait until morning. Go now.
Can portal hypertension be cured?
Not yet. Portal hypertension is a complication of liver damage, usually cirrhosis. Current treatments manage the pressure and prevent complications like bleeding and fluid buildup, but they don’t reverse the scarring. The only cure is a liver transplant - which is reserved for those with advanced disease or failing organs.
How often should I get screened for varices?
If you’ve been diagnosed with cirrhosis, you should have an upper endoscopy to check for varices once. If none are found, repeat every 2 years. If small varices are present, repeat every 1 to 2 years. If you’re on beta-blockers and your varices are gone, your doctor may extend the interval. Always follow your hepatologist’s advice - guidelines vary based on your risk.
Are non-selective beta-blockers safe if I have asthma?
They’re generally avoided in people with active asthma or severe COPD because they can trigger bronchospasm. Alternatives like carvedilol may be used cautiously, or endoscopic banding becomes the main prevention tool. Always discuss your breathing history with your doctor before starting any beta-blocker.
Can I drink alcohol if I have portal hypertension?
Absolutely not. Alcohol accelerates liver damage, increases portal pressure, and raises your risk of bleeding and infection. Even small amounts can be harmful. Complete abstinence is required for anyone with portal hypertension, regardless of the cause.
How long does it take to recover after a TIPS procedure?
Most people go home within 1 to 3 days after TIPS. You’ll feel better quickly - swelling reduces, breathing improves. But full recovery takes weeks. You’ll need regular monitoring for hepatic encephalopathy, which can develop in the first month. Avoid heavy lifting for 2 weeks. Follow-up imaging is needed at 1 month and then every 6 months to check that the shunt stays open.
What’s the survival rate with portal hypertension complications?
It depends. If you have bleeding varices and get prompt treatment, your 6-week survival is about 80%. But if you develop hepatorenal syndrome or recurrent bleeding despite treatment, survival drops sharply - to under 50% within a year. Liver transplant dramatically improves long-term survival. Without it, most people with advanced complications live 1 to 3 years after their first major event.
What Comes Next?
If you’re managing portal hypertension, your next step isn’t just about medicine - it’s about planning. Talk to your hepatologist about:- Whether you’re a candidate for transplant evaluation
- If non-invasive pressure monitoring is available at your center
- How to recognize early signs of encephalopathy or kidney trouble
- Support resources - counseling, nutritionists, patient groups
Portal hypertension doesn’t care if you’re busy, tired, or scared. It waits. But with the right knowledge and care, you can outmaneuver it. Stay vigilant. Stay informed. And don’t let silence be your enemy.





Arlene Mathison January 19, 2026
Just read this and I’m crying. My mom had cirrhosis and we didn’t know how fast things could spiral. She ignored the beta-blockers because she ‘felt fine.’ One day she vomited blood at breakfast. We got there in 20 minutes but it was too late. Please, if you’re reading this - take your meds. Even on the days you feel okay. 💔
clifford hoang January 19, 2026
They say it’s cirrhosis but what if the real cause is glyphosate in our food supply? 🌱💀 Big Pharma doesn’t want you to know that the liver doesn’t ‘scar’ - it’s being chemically sabotaged by the USDA-approved poison in your Cheerios. HVPG? More like ‘Hypnotized by Vague Pseudoscience.’ The SmartBand? A distraction. The real cure is raw liver juice and cold plunges. 🤯
Emily Leigh January 20, 2026
Ugh. Another ‘medical advice’ essay. I mean, really? Salt restriction? Diuretics? Band ligation? Do they even know how many people just… give up? I have ascites. I’m 52. I eat ramen. I don’t care anymore. 😴
Shane McGriff January 22, 2026
I’ve been a nurse for 18 years, and this is one of the clearest, most accurate summaries I’ve ever seen. Especially the part about TIPS and encephalopathy - that trade-off is brutal but real. I’ve seen patients go from bed-bound to walking again after TIPS… then crash two weeks later because no one caught the early confusion. Please, if you’re a caregiver - learn the signs. It’s not ‘just aging.’ It’s liver failure whispering. 🫂
Carolyn Rose Meszaros January 23, 2026
Thank you for writing this. I’ve been living with NAFLD for 5 years and I’ve been terrified to get checked. This made me feel less alone. I’m scheduling my endoscopy next week. You’re right - silence is the enemy. 💪❤️
Paul Barnes January 24, 2026
There is a grammatical error in the third paragraph: ‘That’s scarring. That’s your liver turning stiff, like a dried-out sponge. Blood can’t flow through easily. The rest? Non-cirrhotic causes - things like blood clots…’ - the use of ‘The rest?’ is not a complete sentence and violates standard English syntax. Please correct. Also, ‘HVPG’ should be defined on first use, not assumed. Precision matters.
Art Gar January 24, 2026
While the medical content is largely accurate, I must emphasize that the normalization of non-alcoholic fatty liver disease as an inevitable consequence of modern life is ethically irresponsible. The author implies passivity - ‘manage it’ - when the real solution is personal accountability. No one develops cirrhosis without choosing poor diet, sedentary behavior, and denial. This article is a disservice to those who still have agency. The liver is not a victim. It is a mirror.
pragya mishra January 25, 2026
Why are you all ignoring the real issue? In India, we see portal hypertension in people who don’t even drink. It’s the pesticides in the water. And you think beta-blockers fix that? No. We need clean water. Not more pills. You Americans are so focused on your gadgets and drugs - you miss the root. 🌍💧
Greg Robertson January 26, 2026
Hey, I just wanted to say I really appreciate how you included the emotional stuff - the fear, the exhaustion. My dad’s in stage 4 and he won’t talk about it. This post gave me something to share with him. Not a lecture. Just… truth. Thanks.
Nadia Watson January 27, 2026
I'm so grateful for this post. As a transplant coordinator, I see too many people wait until it's too late. The AI models you mentioned? We're using them now at my hospital. They flagged a patient last month who had zero symptoms - but the algorithm saw the pattern in his voice tone and lab trends. He got a banding session before he bled. That's hope. That's progress. Keep sharing this. 🙏