Diarrhea isn’t just a bad day at the bathroom-it’s a signal. Something in your gut is off. And whether it lasts a day or a month makes all the difference in how you treat it. Most people think of diarrhea as something you just power through with Imodium and rest. But that’s where things go wrong. Using the same approach for a 2-day bug and a 6-month problem can be dangerous. The real key isn’t just stopping the loose stools-it’s understanding why they’re happening.
What Exactly Is Diarrhea?
Diarrhea means three or more loose or watery stools in a day. It’s not about frequency alone-it’s about consistency. If your poop is mushy, watery, or doesn’t hold shape, and it’s happening often, that’s diarrhea. Doctors measure it by stool weight: over 200-300 grams per day. But you don’t need a scale to know. You just know when it’s not normal. The biggest mistake people make? Treating all diarrhea the same. That’s like using a bandage for a broken bone. The cause, duration, and risks change completely depending on how long it lasts.Acute Diarrhea: The Short-Term Bug
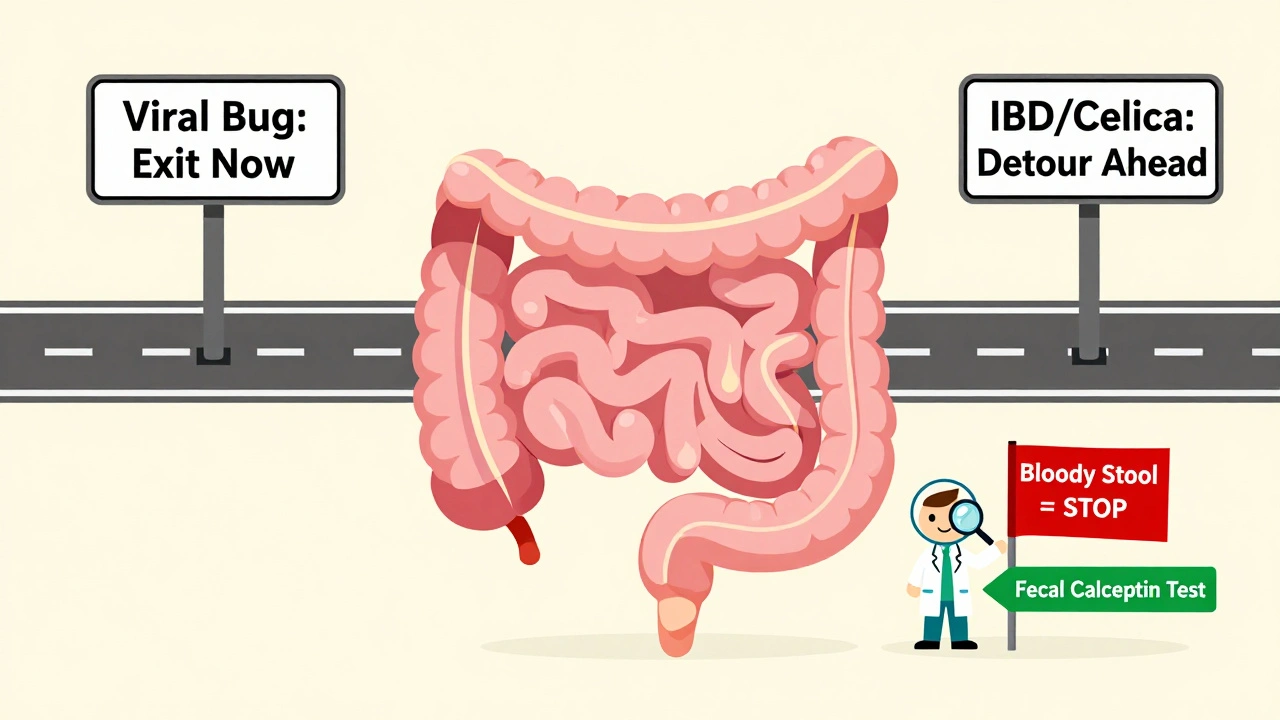
If your diarrhea started suddenly and lasted less than two weeks, you’re dealing with acute diarrhea. This is the kind you get after eating bad sushi, traveling abroad, or catching a stomach virus from your kid. It’s not a disease-it’s a symptom. And in most cases, it’s your body flushing out something harmful. About 70-80% of acute cases in places like Canada or the U.S. are viral. Rotavirus used to be the top culprit, especially in kids. But thanks to vaccines, those cases have dropped by 40-60%. Now, it’s more often norovirus, adenovirus, or just a random bug. Bacteria like Campylobacter or Salmonella cause about 10-20% of cases. Parasites like Giardia show up less often but stick around longer if untreated. You’ll usually feel it fast: cramps, urgency, maybe a low fever. Most people feel better in 3-5 days. In 90% of cases, it clears up on its own without antibiotics. That’s right-antibiotics won’t help most viral cases and can even make things worse by killing off good gut bacteria.Chronic Diarrhea: The Hidden Problem
Now, if your loose stools have been going on for more than 14 days-especially if it’s been months-you’re in the chronic diarrhea zone. This isn’t a bug. It’s a sign of something deeper. About 5% of adults in developed countries deal with this. And most of them wait months before getting a real diagnosis. The causes here aren’t infectious. They’re internal. Think:- Inflammatory Bowel Disease (IBD): Crohn’s or ulcerative colitis. Inflammation in the gut lining leads to constant loose stools, sometimes with blood.
- Irritable Bowel Syndrome (IBS-D): No inflammation, but your gut is hypersensitive. Stress, food triggers, and nerve misfires cause diarrhea. It’s common, affecting 10-15% of people worldwide.
- Bile Acid Malabsorption: After gallbladder removal, bile flows unchecked into the colon and acts like a laxative. About 1 in 4 people who’ve had their gallbladder out get this.
- Medication Side Effects: Antibiotics, metformin, laxatives, even some heart meds can cause chronic diarrhea.
- Celiac Disease: Your body reacts to gluten by damaging the small intestine. Many people are misdiagnosed with IBS for years before testing for this.
Antimotility Agents: When They Help-and When They Hurt
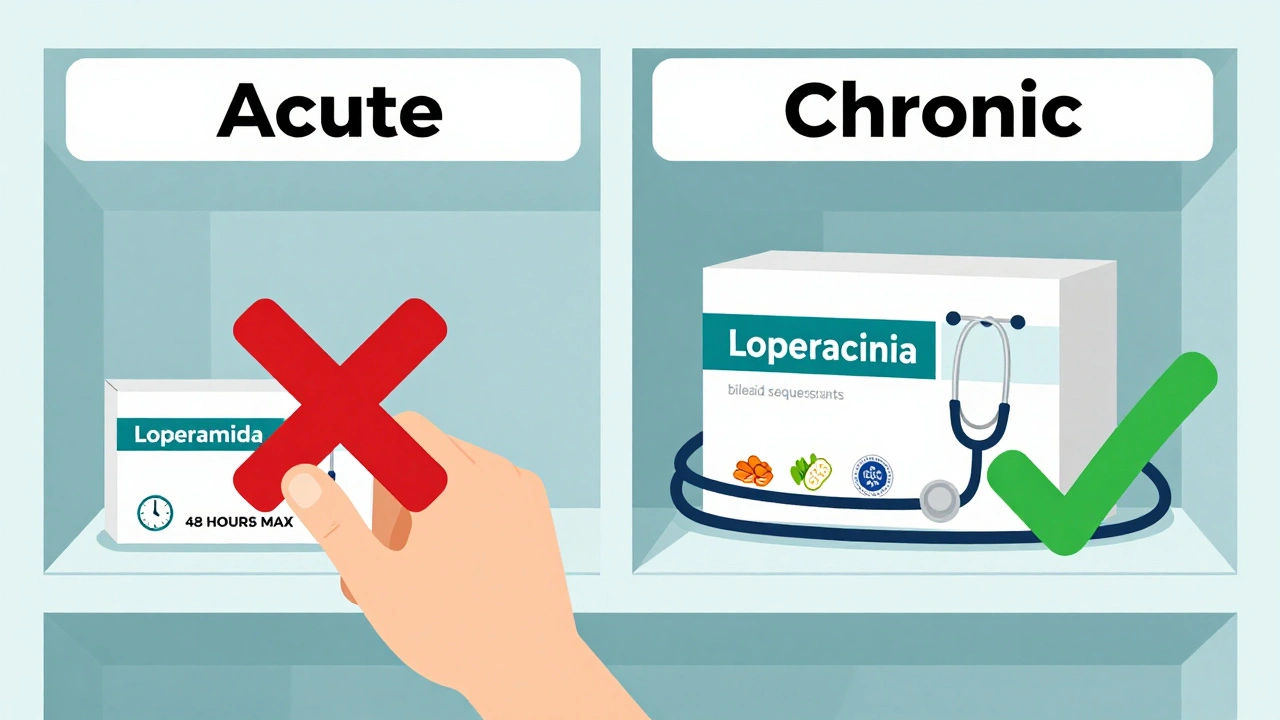
Loperamide (Imodium) is the most common antimotility drug. It slows down gut movement, letting your body absorb more water and firm up stool. It works. But it’s not a cure. It’s a bandage. For acute diarrhea, loperamide can help you get through a workday or a flight. Start with 4mg after the first loose stool, then 2mg after each subsequent one. Don’t go over 16mg in 24 hours. It’s safe for most adults when used short-term. For chronic diarrhea, it’s often part of the plan-especially for IBS-D. Many people find relief taking 2mg before meals. Some need 4-6mg daily. But here’s the catch: over time, tolerance can build. One patient on Reddit said they went from 2mg to 8mg daily just to feel normal. That’s not normal. Here’s the danger zone: Never take loperamide if you have:- Bloody stools
- High fever (over 38.5°C)
- Signs of infection like severe abdominal pain
What You Should Do Instead of Just Reaching for Imodium
For acute diarrhea, skip the BRAT diet. Bananas and toast won’t fix you. The CDC and American College of Gastroenterology now recommend eating normally as soon as you can tolerate it. Focus on fluids. Oral rehydration solution (ORS) is the gold standard. It’s not just water-it’s a precise mix of salt, sugar, and potassium. WHO’s formula: 2.6g sodium chloride, 2.9g trisodium citrate, 1.5g potassium chloride, and 13.5g glucose per liter of water. It cuts death risk from diarrhea by 93% in kids. Even in rich countries, it’s the smartest thing you can do. For chronic diarrhea, you need answers. Not just relief. Ask your doctor for:- Complete blood count (CBC)
- C-reactive protein (CRP)
- Fecal calprotectin (to check for gut inflammation)
- Thyroid function test
- Celiac panel (anti-tTG antibodies)
- Colonoscopy if you’re over 50 or have warning signs
The Bigger Picture: Why This Matters
Globally, diarrhea kills over 500,000 children every year-second only to pneumonia. In the U.S., it costs $2.8 billion annually in medical bills and lost work. The market for loperamide alone is $1.27 billion a year. But money isn’t the issue. Awareness is. We treat diarrhea like a nuisance. But chronic diarrhea can be the first sign of Crohn’s, cancer, or celiac disease. And loperamide, while helpful, is not harmless. Misuse is rising. The FDA now limits packages to 48mg (24 tablets) to curb abuse. New tools are coming. Extended-release loperamide formulations are being approved to reduce abuse risk. Fecal microbiota transplants are curing recurrent C. difficile in 85-90% of cases. And someday, doctors may use blood or stool biomarkers to match you with the right treatment-no trial and error. Until then, the best advice is simple: don’t ignore it. If it lasts more than two weeks, get checked. If you’re taking loperamide daily for months, talk to your doctor. And if you have blood in your stool or a fever-don’t reach for the pills. Go to the clinic.What to Do Right Now
- If diarrhea started suddenly and you’re otherwise healthy: Drink ORS, eat light meals, rest. Use loperamide only if you need to get through a day. Stop after 48 hours.
- If it’s been over 14 days: Write down your symptoms. Note stool frequency, color, odor, and whether you wake up at night. Track foods that make it worse. Make an appointment with your doctor.
- If you’re taking loperamide daily: Don’t increase the dose on your own. Talk to your doctor about alternatives. You might need testing for IBS, celiac, or bile acid issues.
- If you have kids under 2 with diarrhea: Don’t give loperamide. Use ORS and call your pediatrician.
Is it safe to take loperamide every day for chronic diarrhea?
Loperamide can be used daily under medical supervision for conditions like IBS-D, but it’s not meant for long-term self-treatment. Taking more than 16mg per day increases the risk of heart problems and dependence. If you need more than 8mg daily, you likely need testing for an underlying cause like bile acid malabsorption or celiac disease.
Can chronic diarrhea go away on its own?
Rarely. Most cases of chronic diarrhea are caused by conditions like IBS, IBD, or bile acid issues that don’t resolve without treatment. While some people see improvement with diet changes or stress management, persistent symptoms mean you need a diagnosis-not just symptom control.
What’s the difference between watery and fatty diarrhea?
Watery diarrhea is usually secretory or functional-caused by IBS, infections, or medication. Fatty diarrhea, or steatorrhea, means your body can’t digest fat properly. It’s oily, floats, smells terrible, and often comes from pancreatic insufficiency, celiac disease, or bile acid problems. The treatment is completely different.
Why do I get diarrhea after gallbladder removal?
Without a gallbladder, bile flows continuously into your small intestine instead of being stored and released after meals. Too much bile in the colon acts like a laxative. This is called bile acid malabsorption and affects 25-30% of people after gallbladder surgery. It’s treatable with bile acid sequestrants like cholestyramine.
Should I take probiotics for diarrhea?
For acute diarrhea, especially from antibiotics, certain strains like Lactobacillus rhamnosus GG can shorten duration by about a day. For chronic diarrhea, evidence is weaker. Probiotics won’t fix IBS or celiac. They’re not a cure-all-just a possible helper in specific cases.
When should I go to the ER for diarrhea?
Go to the ER if you have bloody stools, high fever (over 39°C), severe abdominal pain, signs of dehydration (dry mouth, dizziness, no urine for 8+ hours), or if you’re over 65 with chronic illness. These aren’t normal symptoms-they’re warning signs.






val kendra December 4, 2025
Just had a 3-week bout of this after a trip to Mexico. Went to the doc, turned out to be bile acid malabsorption. Cholestyramine changed my life. No more panic attacks before leaving the house. Seriously, if you've had chronic diarrhea after gallbladder removal, don't ignore it. It's not 'just stress'.
Elizabeth Crutchfield December 5, 2025
i had no idea loperamide could be abused like that… thought it was just for bad tummy days. now im scared i used too much last winter. 🤢
Chad Handy December 6, 2025
Look, I get that you’re trying to be helpful, but this whole post feels like a medical textbook with a Reddit filter. People don’t come here for CDC guidelines. They come because they’re desperate, embarrassed, and Google gave them 47 different diagnoses. The real problem isn’t loperamide misuse-it’s that primary care doctors won’t take chronic diarrhea seriously until someone collapses. I’ve been told ‘it’s just IBS’ for 8 years. Turns out I had Crohn’s. You think I wanted to spend 3 years in pain while my colon turned to mush? No. You think I wanted to self-medicate with Imodium because I couldn’t get an appointment for 6 months? Yes. So stop lecturing. Start listening.
John Filby December 8, 2025
Wait so if you have fatty diarrhea after gallbladder removal, is that why my poop looks like oil slicks on the toilet? 😅 I thought I was just eating too much cheese. Also, is cholestyramine gross? I heard it tastes like chalky mud.
Shofner Lehto December 9, 2025
For anyone reading this and thinking 'I'll just keep taking Imodium'-stop. It’s not a lifestyle product. I’ve seen patients on 12mg/day for 2 years. Then they show up in the ER with QT prolongation and a heart rate of 150. You don’t need to be an addict to get hurt. Just someone who didn’t know better. Get tested. Your gut is trying to tell you something.
Ashley Elliott December 9, 2025
Thank you for writing this. So many people think diarrhea is 'just a stomach bug'-and then they ignore it for months. I had celiac for 5 years before diagnosis. Thought I had 'stress IBS.' Turns out, eating a single slice of pizza was slowly destroying my intestines. The moment I went gluten-free? My energy came back. My skin cleared. I stopped waking up at 3 a.m. sweating and panicking about the toilet. It’s not 'in your head.' It’s in your gut. And it deserves real answers.
Isabelle Bujold December 11, 2025
Let me just say this: if you’re reading this because you’ve been having loose stools for more than two weeks, please don’t scroll past this thinking 'I’ll deal with it later.' Chronic diarrhea isn’t a nuisance-it’s a red flag. I’m a nurse in Toronto, and I’ve seen too many cases where patients come in with weight loss, night sweats, and bloody stools, and they say, 'I thought it was just food poisoning.' No. It’s not. It’s Crohn’s. It’s lymphoma. It’s microscopic colitis. It’s bile acid diarrhea. It’s celiac. And yes, it can be treated-if you catch it early. I’ve had patients who waited a year because they were embarrassed. One of them ended up in surgery. Don’t be that person. Write down your symptoms. Track your food. Make that appointment. Your future self will thank you.
Ben Choy December 12, 2025
Just wanted to say-ORS is the real MVP. I used to think it was just for kids in developing countries. Then I got sick on a flight and bought a packet at the airport. Tasted like sweet salt water, but within 3 hours, I felt human again. No more dizziness. No more panic. Just… normal. If you’re going to take anything from this post, take this: drink ORS, not just water. It’s science, not folklore.
Emmanuel Peter December 13, 2025
So you're telling me I shouldn't just take Imodium every day because I have IBS-D? Wow. That's a radical idea. I mean, I've been doing it for 7 years and I'm fine. My job requires me to sit in meetings all day. I can't just 'get tested' every time I have a stomach ache. You're not living my life. I'm not going to risk my career because some doctor wants to run 12 different blood tests. I'll keep my 4mg daily. Thanks for the lecture.