PAMORA Comparison Tool
Which PAMORA is best for you?
Answer these questions to find your most appropriate option based on your medical situation
Recommended Option:
Why this option?
Important safety considerations
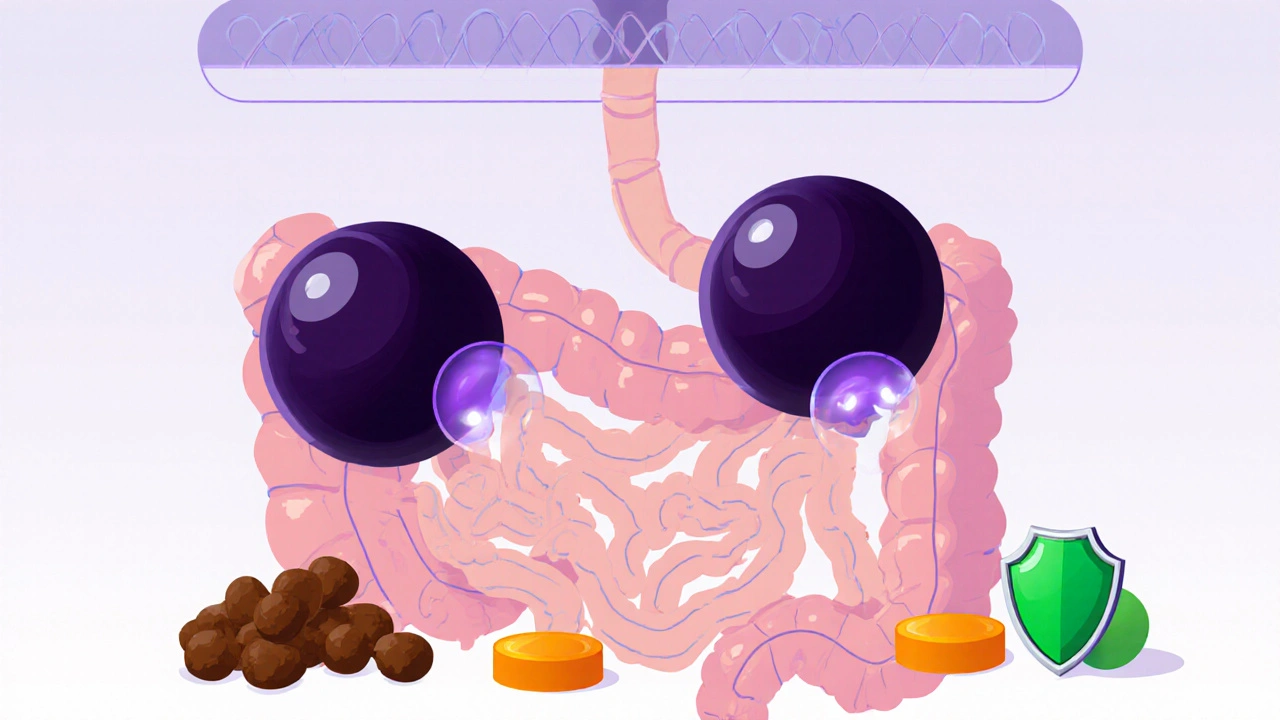
Why Opioids Cause Constipation - And Why Laxatives Often Fail
If you’re taking opioids for chronic pain, you’ve probably noticed something frustrating: no matter how many fiber bars you eat or how much water you drink, your bowels just won’t move. That’s not just bad luck - it’s opioid-induced constipation, or OIC. Up to 80% of people on long-term opioids develop it. And here’s the catch: regular laxatives like senna, magnesium, or even Miralax only help about 30% of the time. Why? Because opioids aren’t just slowing your gut - they’re hijacking the nerves that control it.
Opioids bind to mu-receptors in your intestines, which are everywhere in the gut lining. These receptors normally help regulate digestion, but when opioids lock onto them, they shut down muscle contractions, reduce fluid secretion, and increase water absorption. The result? Hard, dry stools that take days to pass. Traditional laxatives try to force things along, but they don’t touch the root cause: opioid activity in the gut.
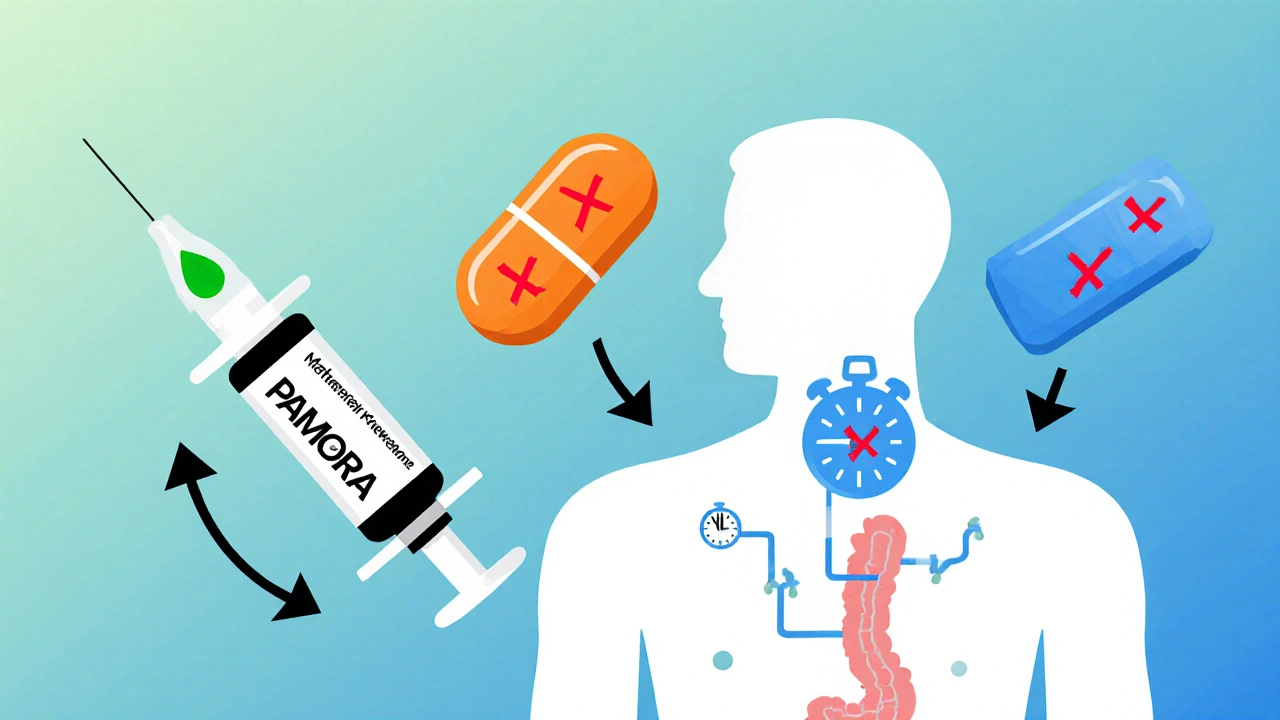
What Are Peripherally Acting Mu Antagonists (PAMORAs)?
PAMORAs are a new kind of drug designed to fix this problem without touching your pain relief. Unlike regular opioid blockers like naloxone, which can reverse pain control entirely, PAMORAs work only in the gut. They’re built to stay out of the brain. That’s because they’re either too large, too charged, or too chemically modified to cross the blood-brain barrier.
There are three main PAMORAs approved in the U.S.: methylnaltrexone (RELISTOR), naloxegol (MOVANTIK), and naldemedine (SYMPROIC). Each has a different chemical structure, but they all do the same thing: block opioid receptors in the intestines while leaving brain receptors alone. This means you keep your pain relief but get your bowels back.
How Each PAMORA Compares: Dosing, Form, and Use
Not all PAMORAs are the same. Here’s how they stack up:
| Drug (Brand) | Form | Dose | Onset of Action | Half-Life | Key Use Case |
|---|---|---|---|---|---|
| Methylnaltrexone (RELISTOR) | Injection or oral tablet | Subcutaneous: 0.15 mg/kg; Oral: 450 mg | 30 minutes to 4 hours | 1.8-2.5 hours | Cancer and noncancer pain patients |
| Naloxegol (MOVANTIK) | Oral tablet | 25 mg daily | 2-4 hours | 8-13 hours | Chronic noncancer pain |
| Naldemedine (SYMPROIC) | Oral tablet | 0.2 mg daily | 1-3 hours | 11-15 hours | Chronic noncancer pain |
Methylnaltrexone is the only one available as an injection - useful for patients who can’t swallow pills or need fast relief. The oral version works well too, especially for home use. Naloxegol and naldemedine are daily pills. Naloxegol needs a lower dose if you have liver problems. Naldemedine is the most forgiving for kidney issues - only avoid it if your kidneys are severely damaged.
How Effective Are They?
Real-world results matter more than lab numbers. In clinical trials:
- Methylnaltrexone helped 52% of patients have a bowel movement within 4 hours - compared to just 30% on placebo.
- Naloxegol led to spontaneous bowel movements in 44% of users after 12 weeks - up from 32% on placebo.
- Naldemedine hit 48% response rate, beating placebo by 13 percentage points.
These aren’t just statistical wins. Patients report real changes: no more straining, no more bloating, no more skipping pain meds just to go to the bathroom. One cancer patient on Reddit said, “RELISTOR let me sleep through the night again. I didn’t realize how much pain constipation was adding.”
Who Shouldn’t Use PAMORAs?
These drugs aren’t for everyone. You should avoid them if you have:
- A blocked intestine (mechanical obstruction)
- Severe kidney disease (naloxegol is off-limits here)
- A history of bowel surgery or recent abdominal trauma
Alvimopan (ENTREGOR), another PAMORA, is only used in hospitals after bowel surgery because of heart risks. It’s not approved for ongoing OIC. Also, don’t take PAMORAs with other opioid blockers - it could cause withdrawal symptoms or sudden pain spikes.
Cost, Access, and Real Patient Experiences
Here’s the tough part: PAMORAs are expensive. Without insurance, you’re looking at $5,000 to $6,000 a year. Even with coverage, copays can hit $300-$450 a month. That’s why many patients stop using them after a few weeks - especially if they don’t see immediate results.
On Drugs.com, methylnaltrexone has a 5.8/10 rating. Naloxegol scores 6.2/10. Common complaints? Abdominal cramps (32% of negative reviews), and “it stopped working after two weeks.” One 67-year-old with osteoarthritis wrote: “I paid $450 a month for nothing.”
But cancer and palliative care patients have a different story. In online support groups, 65% say methylnaltrexone “changed my life.” Why? Because for them, quality of life isn’t theoretical - it’s survival. If you can’t sit comfortably, eat, or sleep, even a small win matters.
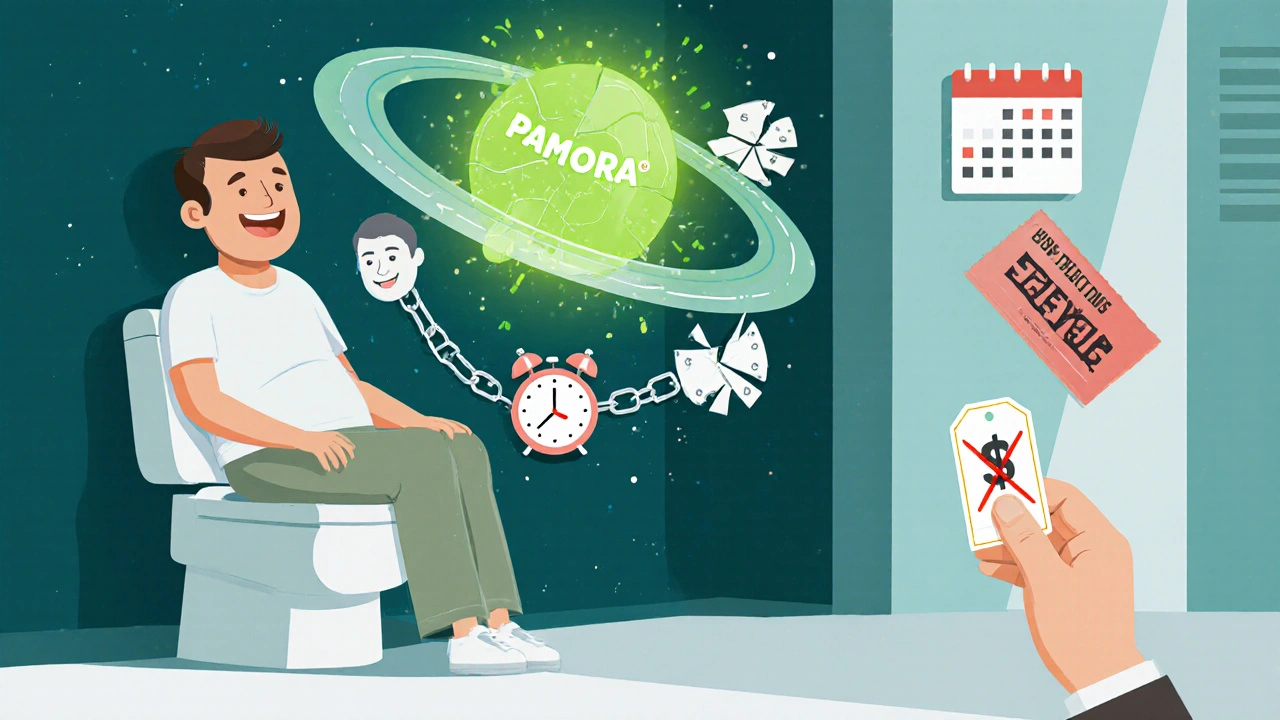
How to Use PAMORAs Right
Getting the timing right makes a big difference. Most doctors start with the lowest dose and adjust slowly. For oral PAMORAs, take them about an hour before your regular opioid dose. That way, when the opioid peaks in your system, the PAMORA is already blocking gut receptors.
Don’t expect miracles on day one. It can take 2-3 weeks to find the right dose. In a survey of 250 pain specialists, 78% admitted they initially underdosed patients. That’s a common mistake - patients give up too soon.
Also, don’t stop your other bowel habits. Keep drinking water, eating fiber, and moving. PAMORAs help, but they’re not magic. Think of them as a tool to restore normal function, not replace healthy habits.
The Future of Opioid Constipation Treatment
Researchers are already working on the next generation. A new dual-action drug - combining a PAMORA with a serotonin booster - is in phase 2 trials and shows 68% response rates. That’s higher than any current option.
Biosimilars are coming too. The first methylnaltrexone biosimilar is in phase 3 trials in China. If approved in the U.S., it could cut costs by 30-50%. But until then, access remains limited. The American Gastroenterological Association warns that without price drops, only 35-40% of people who need PAMORAs will ever get them.
Meanwhile, non-opioid pain treatments are growing. But for now, if you’re stuck between pain control and constipation, PAMORAs are still the most targeted solution we have.
When to Talk to Your Doctor
If you’ve been on opioids for more than a few weeks and haven’t had a bowel movement in 3 days - even with laxatives - it’s time to bring up PAMORAs. Don’t wait until you’re in pain from bloating or vomiting. Ask specifically about methylnaltrexone, naloxegol, or naldemedine. Bring up cost concerns - many manufacturers offer coupons or patient assistance programs.
And remember: your constipation isn’t your fault. It’s a known side effect of the medicine you need. You deserve relief - and there’s a drug designed exactly for that.






Malia Blom November 7, 2025
So let me get this straight-we’re paying $5k a year to un-f*ck a system that opioids broke in the first place? Brilliant. We’re not fixing pain management, we’re just patching the leak while the whole damn boat sinks. 🤡
Erika Puhan November 8, 2025
The pharmacokinetic profile of PAMORAs demonstrates a targeted peripheral antagonism of μ-opioid receptors, thereby circumventing central nervous system-mediated analgesic interference. However, the cost-benefit ratio remains clinically suboptimal in non-oncological populations due to subthreshold efficacy thresholds and high out-of-pocket burden.
Edward Weaver November 9, 2025
America spends billions on this crap while our hospitals can't even get IV bags on time. You want relief? Stop taking opioids. Or move to Canada. They don’t have this mess.
Lexi Brinkley November 10, 2025
I tried RELISTOR after 6 months of being stuck 😫... first time I pooped in 4 days? I cried. Like, actual tears. 🥹 Thank you science 🙏
Kelsey Veg November 11, 2025
so like... these drugs r supposed to help but my cousin said she got crazy cramps and it didnt even work after a week?? like wtf??
Alex Harrison November 12, 2025
I think people underestimate how much this affects quality of life. I’m on oxycodone for spinal stenosis and without naloxegol, I was basically housebound. Now I can sit through dinner with my grandkids. Small wins matter.
Jay Wallace November 13, 2025
I’ve read the FDA labels. I’ve reviewed the phase 3 trials. I’ve cross-referenced the pharmacoeconomic models. And I can tell you-this is not a ‘miracle cure.’ It’s a Band-Aid on a bullet wound. And the pharmaceutical industry is laughing all the way to the bank. 💸
Alyssa Fisher November 14, 2025
It’s interesting how we’ve engineered a drug that selectively blocks opioid receptors in the gut but not the brain. That’s actually a pretty elegant solution-like a molecular bouncer that only kicks out the troublemakers in the back room. Makes you wonder why it took so long.
Alyssa Salazar November 15, 2025
The 68% response rate on that dual-action drug in phase 2? That’s the future. Serotonin + PAMORA = the holy grail. Why are we still stuck with these half-measures? The science is here. The pharma execs are just dragging their feet.
Beth Banham November 16, 2025
I’m just glad someone finally made something that doesn’t make you feel like you’re being gut-punched every time you take it. I don’t need a miracle. Just a little peace.
Brierly Davis November 18, 2025
If you're thinking about trying one of these, don't give up after a week. My doc said 2-3 weeks to adjust. Took me 3 weeks, but now I'm back to hiking on weekends. You got this 💪
Jim Oliver November 19, 2025
Oh wow, a $450/month pill to fix constipation. Next they’ll sell us a $10,000 spoon to eat with. 😴
William Priest November 21, 2025
I mean... if you’re on opioids long-term, you kinda signed up for this. Why not just eat prunes and get a colonoscopy? Seems less… corporate.
Ryan Masuga November 22, 2025
I know it’s expensive but I’ve seen friends go from 7 days without a BM to daily with naldemedine. It’s not perfect, but it’s a lifeline. Don’t let the price tag make you ignore the real need.
Jennifer Bedrosian November 23, 2025
I went from crying in the bathroom every night to laughing with my kids again thanks to RELISTOR and I’m not even gonna apologize for how emotional this is 🤍