Meglitinides Meal Timing Risk Calculator
When you’re managing type 2 diabetes, timing isn’t just important-it’s life-saving. That’s especially true if you’re taking meglitinides. These drugs work fast, but they don’t wait for you. If you skip a meal, your blood sugar can crash-sometimes in under an hour.
What Are Meglitinides?
Meglitinides are a class of oral diabetes medications designed to help control blood sugar after meals. The two main ones are repaglinide and nateglinide. Unlike metformin, which works by reducing liver sugar production, meglitinides tell your pancreas to release insulin right when you eat. They’re fast-acting: repaglinide starts working in 15 to 30 minutes, and nateglinide even faster-within 1 minute. Peak insulin release happens within an hour, and the effect fades in just 2 to 4 hours.
This quick action makes them ideal for people with unpredictable schedules-someone who eats lunch at 1 p.m. one day and 4 p.m. the next. But that same speed is what makes them dangerous if you don’t eat when you’re supposed to.
The Meal Timing Trap
The whole point of meglitinides is flexibility. You don’t need to take them at the same time every day. You take them 15 minutes before you eat. But if you forget, or if your meal gets delayed, your body is already pumping out insulin with no food to use it.
That’s when hypoglycemia kicks in. Blood sugar drops below 70 mg/dL. Symptoms? Shaking, sweating, dizziness, confusion. In severe cases, it can lead to seizures or loss of consciousness.
Studies show that skipping just one meal after taking a meglitinide increases your risk of low blood sugar by 3.7 times. And it doesn’t take long-within 90 minutes of dosing, your blood sugar can plummet. For older adults or those with kidney problems, the risk is even higher. One study found that patients with advanced chronic kidney disease had a 2.4-fold greater chance of hypoglycemia on meglitinides than those without kidney issues.
How It Compares to Other Diabetes Drugs
Not all diabetes meds work like this. Sulfonylureas-like glipizide or glyburide-also stimulate insulin release, but they stick around for 12 to 24 hours. That means you can get low blood sugar even if you haven’t skipped a meal. Meglitinides are different. Their danger is tied directly to meal timing.
Repaglinide is slightly more effective at lowering HbA1c than nateglinide, but it also causes about 28% more episodes of hypoglycemia. That’s a trade-off: better control, but more risk. And if you’re on insulin or another insulin-stimulating drug, the risk multiplies. Combining meglitinides with sulfonylureas or insulin can lead to dangerous, overlapping insulin spikes.
For people with kidney problems, repaglinide has an advantage. It’s mostly broken down by the liver, not the kidneys. That’s why guidelines recommend it over sulfonylureas for those with low kidney function-though even then, the dose needs to be cut in half (60 mg instead of 120 mg) if your kidney filter rate drops below 30 mL/min.

Real-World Risks
Most hypoglycemia events with meglitinides happen between 2 and 4 hours after taking the pill. That’s the peak window-when insulin is highest and food is either delayed or missing. In real life, this happens often. People get busy. They lose track of time. They skip breakfast because they’re running late. They eat dinner late after a long day.
One study found that 41% of all low blood sugar episodes in meglitinide users occurred during this exact window. And it’s not just about forgetting meals. Cognitive decline, depression, or simply living alone can make regular eating harder. The American Diabetes Association’s 2025 guidelines specifically warn that older adults are at higher risk because of “irregular meal intake.”
How to Stay Safe
If you’re on meglitinides, your safety depends on two things: consistency and awareness.
- Take it only when you’re about to eat. Never take it if you’re unsure whether you’ll eat in the next 15 to 30 minutes. This is called the “dose-to-eat” approach. It’s safer than taking it on a fixed schedule.
- Carry fast-acting sugar. Keep glucose tablets, juice, or candy with you at all times. If you feel shaky or sweaty, act fast.
- Don’t skip meals. Even a missed snack can trigger a drop. If you know you won’t eat for hours, skip the dose.
- Use reminders. Smartphone apps that send pre-meal alerts have been shown to cut hypoglycemia events by 39% in people with irregular schedules.
- Consider CGM. Continuous glucose monitors (CGMs) track your blood sugar in real time. For meglitinide users, studies show CGMs reduce low blood sugar episodes by 57%.
It’s not about being perfect. It’s about being prepared. If you’re traveling, eating out, or working odd hours, plan ahead. Talk to your doctor about adjusting your schedule. Maybe you need a different medication.
Who Should Avoid Meglitinides?
They’re not for everyone. If you have:
- Very unpredictable eating habits with no way to track them
- History of severe hypoglycemia
- Cognitive issues that make meal timing hard
- Already on insulin or sulfonylureas
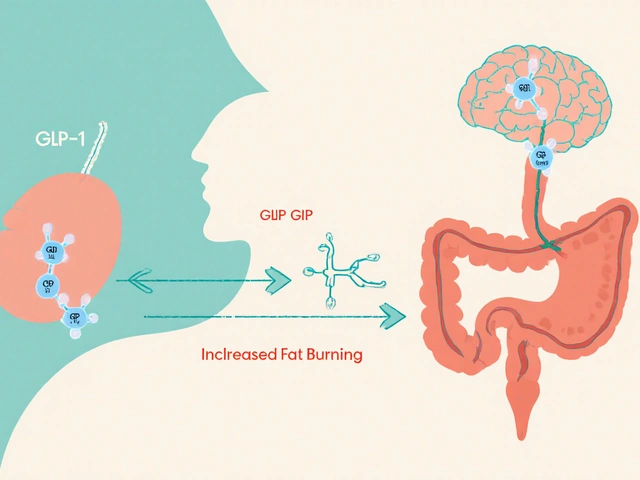
…then meglitinides might not be the best choice. Newer drugs like GLP-1 agonists (such as semaglutide) have a much lower risk of low blood sugar-unless they’re combined with insulin secretagogues. That’s why many doctors now turn to them first for older patients or those with irregular routines.
The Bigger Picture
Meglitinides make up only about 4.2% of oral diabetes prescriptions in the U.S. They’re not first-line. Metformin is. SGLT2 inhibitors and GLP-1 agonists are growing fast. But meglitinides still have a place-for people who need that quick, meal-triggered insulin boost and can’t take injections.
Pharmaceutical companies are working on solutions. A new extended-release version of repaglinide is in Phase II trials. Early results show 28% fewer hypoglycemia events compared to the standard version. That could change the game.
But until then, the rule stays the same: take meglitinides only when you’re about to eat. No exceptions. No shortcuts. Your pancreas doesn’t know you’re busy. It just releases insulin. And if there’s no food, your body pays the price.
Can I take meglitinides if I skip meals often?
No, not safely. Meglitinides are designed for people who can coordinate meals with doses. If you frequently skip meals or eat at random times, these drugs increase your risk of dangerous low blood sugar. Talk to your doctor about alternatives like GLP-1 agonists or SGLT2 inhibitors, which don’t rely on meal timing.
What should I do if I forget to take my meglitinide before eating?
If you realize you missed your dose right after eating, take it immediately. If it’s been more than 30 minutes since you started eating, skip the dose. Don’t double up later. Taking it too late increases the risk of hypoglycemia because the drug will peak when your blood sugar is already dropping.
Is repaglinide safer than nateglinide for kidney patients?
Yes. Repaglinide is mainly processed by the liver, not the kidneys, making it the preferred meglitinide for people with chronic kidney disease. However, the dose must be reduced to 60 mg per meal if your kidney function is below 30 mL/min/1.73m². Nateglinide is cleared by the kidneys, so it’s riskier in advanced kidney disease.
Can I drink alcohol while taking meglitinides?
Alcohol increases the risk of hypoglycemia and can mask its symptoms-like dizziness or confusion-making it harder to recognize a low blood sugar episode. Avoid alcohol, especially on days when your meals are irregular. If you do drink, always eat food with it and monitor your blood sugar closely.
Do I need a continuous glucose monitor (CGM) if I’m on meglitinides?
Not everyone, but if you have irregular meals, are over 65, or have had low blood sugar before, a CGM is strongly recommended. Studies show it cuts hypoglycemia episodes by 57% in meglitinide users. It gives you real-time alerts so you can eat before your blood sugar crashes.
Are there any new meglitinide options coming soon?
Yes. A longer-acting version of repaglinide (repaglinide XR) is in late-stage trials. Early results show it reduces hypoglycemia by 28% compared to the standard form, while still allowing flexible dosing. If approved, it could make these drugs safer for people with unpredictable schedules-but it’s not available yet.
Final Thought
Meglitinides are powerful tools-but they’re not forgiving. They demand precision. If your life is chaotic, your medication shouldn’t add to the risk. Talk to your doctor. Consider alternatives. Or if you stick with meglitinides, make meal timing non-negotiable. Your body doesn’t care how busy you are. It only knows: insulin released, food missing = danger.






Adewumi Gbotemi January 11, 2026
Man, this is so real. In Nigeria, a lot of folks skip meals because food isn't always on time, and then they wonder why they feel weak. This post saved my cousin's life-he was on repaglinide and kept passing out. Now he uses phone alarms and carries juice everywhere. Simple stuff, but it works.
Priya Patel January 12, 2026
OMG I just realized I’ve been doing this wrong 😳 I take my nateglinide before I leave for work and hope I eat later… no wonder I get dizzy by 2pm. Time to fix this before I pass out at my desk again.
Michael Patterson January 13, 2026
So basically if you’re not a robot who eats at 8 12 and 6 every day you shouldnt even be on these drugs? Wow. So the drug companies just made a medication that only works for people with perfect lives? Classic. Also i think they forgot to mention that most people cant afford cgms so good luck with that advice lol.
Jennifer Littler January 14, 2026
From a clinical pharmacology standpoint, meglitinides’ pharmacokinetics are uniquely vulnerable to meal timing due to their rapid absorption and short half-life (t1/2 ~1 hour for repaglinide). The hepatic metabolism via CYP3A4 means drug interactions (e.g., with azoles or macrolides) can amplify hypoglycemic risk beyond meal omission alone. The 3.7x risk multiplier cited is consistent with the UKPDS subanalysis of meal-skipping events. Clinically, this class is best reserved for patients with preserved renal function and structured eating patterns-otherwise, the risk-benefit ratio tilts unfavorably. CGM integration is not optional; it’s standard of care for this cohort.
Madhav Malhotra January 15, 2026
In India, we have so many people who skip meals because of work or family obligations. I’ve seen my uncle take his medicine and then not eat for 5 hours because his shift got delayed. He ended up in the ER. This article? It’s a lifeline. We need more of this in local languages.
Alex Smith January 16, 2026
Oh wow, so the solution to a drug that’s dangerous when you’re busy is… to be less busy? Groundbreaking. Next you’ll tell me that if you’re poor, you should just buy more organic kale and start meditating. Real helpful. Also, why is everyone acting like CGMs are just lying around at CVS? They cost $500 a month. Most people on these meds can’t even afford insulin, let alone a fancy watch that beeps.
Matthew Miller January 17, 2026
This is why people die from diabetes. Not because of the disease-because of lazy doctors prescribing these time-sensitive drugs to people who can’t even set a phone alarm. You’re not a toddler. You can’t just wing it with insulin. This isn’t a game. Stop pretending your chaotic life is an excuse. The drug doesn’t care if you’re tired. Neither does your pancreas. You’re lucky you’re still alive.
Priscilla Kraft January 17, 2026
Just wanted to say thank you for writing this. I’m 68, live alone, and have kidney issues. My doc switched me to repaglinide 60mg because of my eGFR, and honestly? I was terrified. But now I use my Alexa to say ‘REMINDER: Eat now!’ every day at noon and 6pm. I keep juice in my purse and my CGM on 24/7. It’s not perfect, but I’m alive. And I’m not alone. 💙
Jason Shriner January 19, 2026
So let me get this straight… if you’re human, you’re not supposed to take this drug? Because apparently the only people who can use meglitinides are the ones who have a personal chef, a life coach, and a PhD in time management. Meanwhile, the rest of us are just… guilty of existing. Thanks for making us feel like failures for having a Tuesday.
Roshan Joy January 19, 2026
I’m a nurse in Mumbai, and I’ve seen this play out too many times. Patients take their pills and then go back to work because they can’t afford to stop. One lady told me, ‘I skip meals every day. What else can I do?’ This isn’t about discipline-it’s about systems failing people. We need cheaper CGMs, community health workers who check in, and doctors who actually listen. This post is great, but the real fix is bigger than a pill.
Sean Feng January 20, 2026
Just take metformin and stop being dramatic