Heel pain that hits hardest when you first step out of bed? You’re not alone. About 10% of adults will deal with plantar fasciitis at some point in their lives, and it’s the top reason people visit doctors for foot problems. But here’s the twist: it’s not really an inflammation. Doctors now call it plantar fasciopathy - a degenerative wear-and-tear condition that slowly breaks down the thick band of tissue running along the bottom of your foot, from heel to toes. This tissue, the plantar fascia, holds up your arch and absorbs shock with every step. When it starts to fray, pain follows - sharp, stabbing, and stubborn.
Why Your Heel Hurts in the Morning
The classic sign? Pain so bad during your first five steps after waking up that you almost limp. That’s not just bad luck. Overnight, your plantar fascia tightens up. When you stand, it’s suddenly stretched too far, too fast. The result? A flare-up at the point where the tissue attaches to your heel bone. By the time you’ve walked around for 10 minutes, the pain eases - but it comes back after standing all day, or after sitting for a while. Most people rate the pain between 6 and 8 out of 10 when it’s at its worst.
It’s not just runners who get this. In fact, 63% of cases happen in people who are mostly sedentary but carry extra weight - a BMI over 27 increases your risk by more than four times. The other 37% are active - long-distance runners, dancers, or people on their feet all day. Teachers, nurses, and factory workers are especially at risk. If you’re on your feet more than four hours a day, your odds jump by over five times.
What Doctors Look For
There’s no single test that confirms plantar fasciopathy. Diagnosis is based on symptoms and physical checks. Your doctor will press about two to three centimeters forward from the inside of your heel - that’s where the pain usually spikes. They’ll also ask if you have pain when you pull your toes up toward your shin. If you do, that’s a strong clue. An ultrasound can show if the plantar fascia is thicker than normal - over 4.0 mm instead of the usual 2.0 to 3.5 mm. That’s a clear sign of damage.
And here’s something many people don’t know: heel spurs don’t cause this pain. X-rays might show a bony growth on the heel, but 80% of people with plantar fasciopathy have no spurs at all. Meanwhile, 15% of people with no pain at all have spurs on their X-rays. So if your doctor immediately orders an X-ray and tells you the spur is the problem - they’re missing the real issue.
What’s Not Plantar Fasciitis
Not all heel pain is the same. Some people have burning or tingling pain on the inside of the heel - that could be nerve entrapment, like Baxter’s neuritis or tarsal tunnel syndrome. These conditions affect the nerves, not the fascia. The pain feels different - more electric or numb - and doesn’t follow the same pattern as plantar fasciopathy. If stretching doesn’t help after a few weeks, or if the pain spreads up your ankle or into your arch, it’s worth checking for nerve issues.

What Actually Works: Evidence-Based Treatments
Eighty to ninety percent of people get better within six to twelve months using conservative methods. The key? Consistency. Most treatments fail because people give up too soon or skip the basics.
1. Plantar Fascia Stretching - The #1 Recommendation
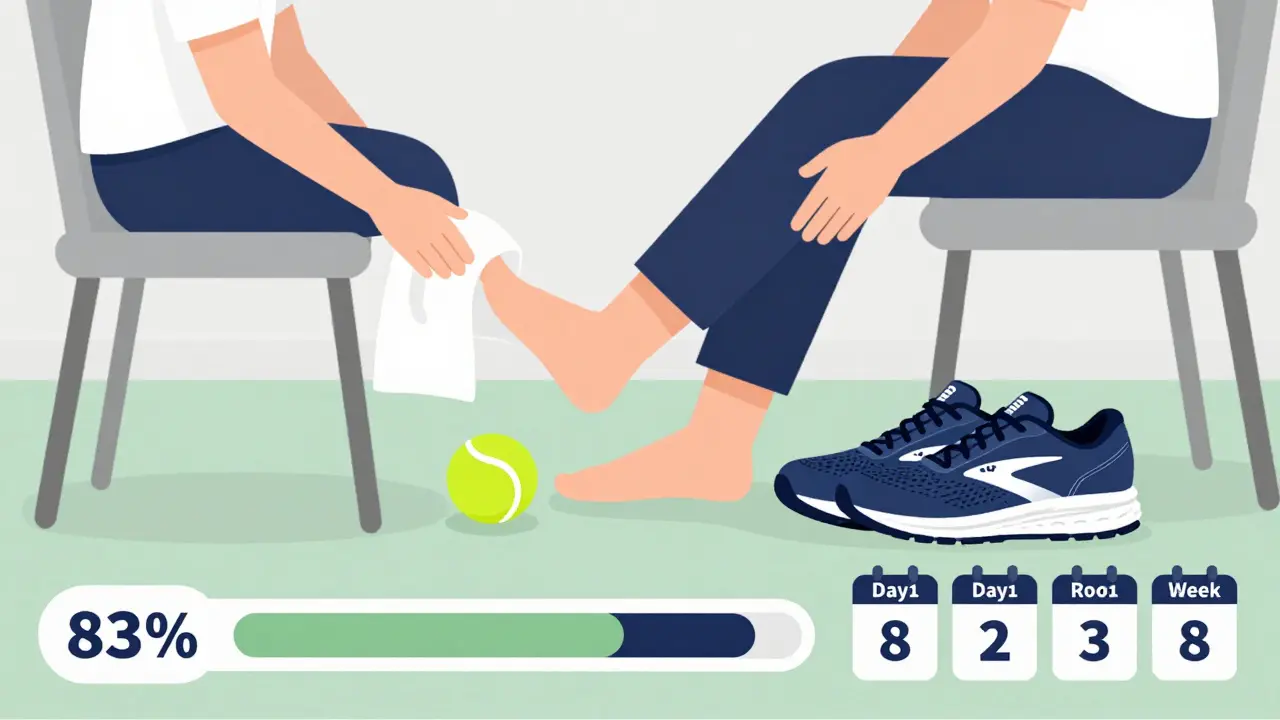
Forget just stretching your calves. The most effective stretch targets the plantar fascia directly. Sit down, cross one leg over the other, and loop a towel around the ball of your foot. Pull your toes gently toward your shin until you feel a stretch along the bottom of your foot. Hold for 10 seconds. Do 10 reps, three times a day. That’s it. No equipment. No cost.
Studies show this specific stretch reduces pain 37% more than regular calf stretches after just four weeks. People who stick with it for 8 to 12 weeks report 83% improvement. One Reddit user, u/RunningHealer, cut his morning pain from 8/10 to 2/10 in six weeks using this method plus rolling his foot on a tennis ball.
2. Night Splints - For Overnight Relief
A night splint keeps your foot at a 90-degree angle while you sleep, preventing the fascia from tightening. Studies show 72% of users see improvement within six weeks - compared to only 45% with a placebo. But here’s the catch: 44% of people quit because the splint is uncomfortable. If you can tolerate it for 4 to 5 hours a night, it’s one of the most effective tools. It works best paired with stretching.
3. Orthotics - Support Matters
Custom orthotics aren’t always necessary. Prefabricated ones work well for most people - they reduce pain by 52%. Custom ones? Just 16% better at 12 weeks. The real difference is in the shoe. Look for ones with a heel-to-toe drop of 10 to 15 mm and good arch support. Models like the Brooks Adrenaline GTS and Hoka Clifton get high satisfaction ratings from users. Avoid flat shoes, flip-flops, or worn-out sneakers - they make things worse.
4. Weight Loss - The Hidden Game-Changer
If your BMI is over 27, losing even a few pounds helps. Research shows each one-point drop in BMI leads to a 5.3% reduction in pain at six months. It’s not about drastic diets - just small, consistent changes. Less pressure on your feet means less strain on the fascia.
Treatments to Avoid or Use Carefully
Not everything sold as a solution actually works - or even helps.
Corticosteroid Injections
They give quick relief - but it’s temporary. On average, pain comes back after 4.2 weeks. Worse, multiple injections carry an 18% risk of rupturing the plantar fascia. They also cause fat pad atrophy - meaning your heel loses its natural cushion. Experts now strongly advise against using them within the first three months. Only consider them if everything else has failed.
Extracorporeal Shockwave Therapy
This non-invasive treatment uses sound waves to stimulate healing. It works for 70-80% of people after 3 to 4 sessions. But it costs $2,500 to $3,500 out-of-pocket, and insurance rarely covers it. It’s a second-line option after 3 months of failed stretching and orthotics.
Platelet-Rich Plasma (PRP) and Cryoplasty
PRP injections - using your own blood - show promise, with 65% pain reduction at six months. But they cost $800 to $1,200 per shot and aren’t covered by insurance. Cryoplasty - freezing the damaged tissue - is still experimental. Don’t waste money on these unless you’ve tried everything else and are willing to pay out-of-pocket.
What Most People Get Wrong
Here’s what stops people from getting better:
- Stretching through pain. If it hurts badly, you’re doing it wrong. You should feel tension, not sharp pain.
- Wearing the wrong shoes. 58% of workplace cases are tied to poor footwear. No more barefoot walking or worn-out sneakers.
- Returning to activity too soon. 72% of recurrences happen because people go back to running or standing too fast.
- Expecting instant results. This isn’t a 2-week fix. You need at least 6 to 8 weeks of daily stretching to see real change. 92% adherence is needed for best results.
Long-Term Outlook
The good news? 90% of people recover fully within 10 months with the right approach. The bad news? About 25 to 30% of people get it back within a year - usually because they stop stretching or gain weight again. Plantar fasciopathy is a lifestyle condition. It responds to habits, not quick fixes.
Think of it like back pain or knee arthritis. You don’t cure it with one treatment. You manage it with daily care: stretching, supportive shoes, weight control, and avoiding overuse. The people who get better are the ones who treat it like a long-term habit - not a short-term problem.
Is plantar fasciitis the same as heel spurs?
No. Heel spurs are bony growths that sometimes appear on X-rays, but they don’t cause the pain. About 80% of people with plantar fasciopathy have no spurs at all, and 15% of people with no pain have spurs. The real issue is damage to the plantar fascia tissue, not the bone.
Can I still run with plantar fasciitis?
You can, but only after symptoms improve and with major adjustments. Reduce mileage, switch to lower-impact activities like swimming or cycling, and make sure you’re wearing proper shoes with support. Never run through sharp pain. Most people need to pause running for 6 to 8 weeks while they focus on stretching and recovery.
How long does it take to heal from plantar fasciitis?
Most people see improvement within 6 to 8 weeks with consistent stretching. Full recovery usually takes 6 to 12 months. The key is sticking with daily stretches - even when the pain eases. Stopping too early is the main reason it comes back.
Do I need custom orthotics?
Not usually. Prefabricated orthotics reduce pain by 52%, and custom ones only add 16% more benefit after 12 weeks. The bigger factor is your shoe. Look for a 10-15mm heel-to-toe drop and good arch support. Brands like Brooks and Hoka are often recommended by users. Save your money unless you’ve tried everything else and still have pain.
Is plantar fasciitis caused by inflammation?
No. It’s now understood as a degenerative condition - called plantar fasciopathy - where the tissue breaks down over time due to overuse. There’s little to no inflammation. That’s why anti-inflammatory drugs like ibuprofen only give short-term relief. The real fix is mechanical: stretching, support, and reducing stress on the tissue.
What to Do Next
Start today. Do the towel stretch three times a day - morning, afternoon, and before bed. Put on supportive shoes as soon as you get up. Avoid walking barefoot. If you’re overweight, aim to lose even 5 pounds - that’s a 25% reduction in foot pressure. Track your pain daily on a scale of 1 to 10. If you don’t see improvement after 6 weeks, see a physical therapist. Most insurance plans cover 80% of physical therapy after your deductible.
Plantar fasciopathy isn’t a life sentence. It’s a signal - your body is asking for better support, more care, and less strain. Listen to it. The tools are simple. The results? Life-changing.






Kevin Motta Top December 20, 2025
Been dealing with this for 3 years. The towel stretch changed everything. Did it religiously for 8 weeks and now I can run again without wincing. No magic pills, just consistency.
Nina Stacey December 20, 2025
i know right like i was so skeptical at first i thought oh great another thing to do but like after i started doing the towel thing three times a day even just while watching tv it got better like not overnight but like gradually and now my morning steps dont feel like stepping on glass anymore honestly if you try this and give it a shot you might be surprised
Janelle Moore December 22, 2025
they dont want you to know this but plantar fasciitis is caused by 5G towers and fluoride in the water theyre hiding the real cure its all about magnetic insoles and drinking apple cider vinegar with cayenne pepper every morning
Henry Marcus December 23, 2025
OMG YES!! I was SO done with this crap-then I found out the ‘spur’ myth is a scam run by Big Orthopedics™. I threw out my expensive custom inserts and bought a $12 tennis ball. Now I roll it under my foot like it owes me money. Life. Changed.
Isabel Rábago December 24, 2025
People who don’t stretch are just lazy. I’ve seen so many of you complain about discomfort but refuse to do the 10-second stretch. You want relief? Then stop treating your body like a disposable machine. This isn’t hard. It’s just discipline. And you’re failing.
Matt Davies December 26, 2025
That night splint thing? I thought I’d never wear it. But I did-just 4 hours a night-and it felt like my foot finally got a good night’s sleep. Still a bit weird, but worth it. Also, Hoka Cliftons are the real MVPs. Don’t let anyone tell you otherwise.
Mike Rengifo December 27, 2025
My dad had this for 15 years. He swore by the tennis ball roll and never wore shoes indoors. Now he’s 72 and walks 5 miles a day. Simple stuff works. You just gotta stick with it.
Dev Sawner December 28, 2025
It is imperative to underscore that the degenerative etiology of plantar fasciopathy is not adequately addressed by superficial interventions such as stretching. The biomechanical load distribution must be quantitatively analyzed through gait studies, and footwear recommendations should be derived from pressure mapping data, not anecdotal user testimonials.
Meenakshi Jaiswal December 28, 2025
Hey, I’m a physio and I see this all the time. The towel stretch works because it targets the fascia directly-not the calf. Most people skip this and wonder why nothing helps. Do it every morning before you even stand up. And yes, weight loss helps, even 5 lbs. You got this. 💪
Connie Zehner December 30, 2025
Wait… so you’re telling me I’m not supposed to wear my Birkenstocks? And my orthotics are useless? And I can’t just take ibuprofen and call it a day? 😭 I’ve been doing everything wrong for TWO YEARS. I’m a mess.
Moses Odumbe December 30, 2025
Bro. I tried the splint. It felt like my foot was in a vice. But I kept it on for 3 nights. On the 4th, I woke up and my heel didn’t scream. I cried. Then I bought 3 more. 🙏
Kelly Mulder December 30, 2025
It is frankly astonishing that this article recommends prefabricated orthotics over custom ones. The lack of scientific rigor here is concerning. One must consider the subtleties of metatarsal alignment, calcaneal inclination angle, and intrinsic foot muscle activation-none of which are addressed by mass-produced insoles. This is pseudoscience dressed as advice.