SGLT2 Inhibitor Risk Assessment Tool
Assess Your Risk
This tool helps you understand your risk of serious infections when taking SGLT2 inhibitors (like canagliflozin, dapagliflozin, empagliflozin) based on your medical history. Results are based on a 2024 study in Diabetes Care.
When you’re managing type 2 diabetes, finding a medication that lowers blood sugar without causing low glucose episodes is a win. That’s why SGLT2 inhibitors became so popular. Drugs like canagliflozin, dapagliflozin, and empagliflozin work by making your kidneys flush out extra sugar through urine. It sounds simple-and it is. But that same mechanism is also why some people end up with unexpected, sometimes serious, yeast and urinary infections.
How SGLT2 Inhibitors Work (and Why They Cause Infections)
SGLT2 inhibitors block a protein in your kidneys that normally reabsorbs glucose. Instead of being pulled back into your bloodstream, sugar gets dumped into your urine. On average, you’ll lose between 40 and 110 grams of glucose per day. That’s like pouring a full soda can’s worth of sugar into your bladder every day.
That sugar doesn’t just disappear. It stays in your urinary tract, creating a sweet, warm, moist environment perfect for yeast and bacteria to grow. It’s not the drug itself causing the infection-it’s the sugar it leaves behind.
Studies show that about 3% to 5% of people taking these medications develop genital yeast infections. For women, that usually means vulvovaginal candidiasis-itching, burning, thick white discharge. For men, it’s balanitis: redness, swelling, and discomfort around the head of the penis. These usually show up within the first few months of starting the drug.
More Than Just Itching: The Real Danger
Most yeast infections are annoying but treatable. But in some cases, what starts as a simple fungal infection can turn into something far worse.
The U.S. Food and Drug Administration (FDA) flagged serious complications as early as 2015. Between March 2013 and October 2014, they recorded 19 cases of urosepsis-bloodstream infections triggered by urinary tract infections-in people taking SGLT2 inhibitors. All 19 required hospitalization. Four needed intensive care. Two needed dialysis because their kidneys failed.
One case from the National Institutes of Health involved a 64-year-old woman who developed emphysematous pyelonephritis-a rare, gas-forming kidney infection-while taking dapagliflozin. She needed surgery and months of antibiotics. Eleven months later, after restarting the drug, she got another kidney infection and a perinephric abscess. She told her doctor: “I never had urinary problems before this medication. Now I’ve had two life-threatening infections.”
These aren’t outliers. The FDA found that infections linked to SGLT2 inhibitors were more likely to be complicated, requiring longer hospital stays and more aggressive treatment than infections in people taking other diabetes drugs.
How Big Is the Risk Compared to Other Drugs?
Let’s put this in perspective. A 2022 meta-analysis compared SGLT2 inhibitors to other common diabetes medications:
- They increased the risk of urinary tract infections by nearly 80% compared to DPP-4 inhibitors, sulfonylureas, and thiazolidinediones.
- For genital infections, the risk jumped over four times higher than with DPP-4 inhibitors.
But here’s the twist: these drugs are still recommended for many people. Why? Because they don’t just lower blood sugar-they protect the heart and kidneys.
In the EMPA-REG OUTCOME trial, empagliflozin reduced the risk of heart-related death by 38% in people with heart disease. Canagliflozin cut major cardiovascular events by 14%. That’s huge. For someone with a history of heart attack or heart failure, the benefits often outweigh the risks.
But if you’ve had recurrent UTIs, kidney stones, or a weakened immune system? That’s a different story. For you, the risk might be too high.

Who Should Avoid SGLT2 Inhibitors?
These drugs aren’t for everyone. You should think twice-or talk to your doctor-before starting one if you have:
- History of frequent or severe urinary tract infections
- Structural problems in your urinary tract (like an enlarged prostate or bladder prolapse)
- History of Fournier’s gangrene (a rare but deadly infection of the genitals and perineum)
- Low kidney function (eGFR below 60 mL/min)
- Are over 65 and female (higher risk due to anatomy and hormonal changes)
- Have an HbA1c above 8.5% (higher sugar levels mean more sugar in urine)
A 2024 study in Diabetes Care created a simple 5-point risk score. If you score 3 or more points, your chance of a serious infection jumps to over 15%. That’s not a small risk. It’s a red flag.
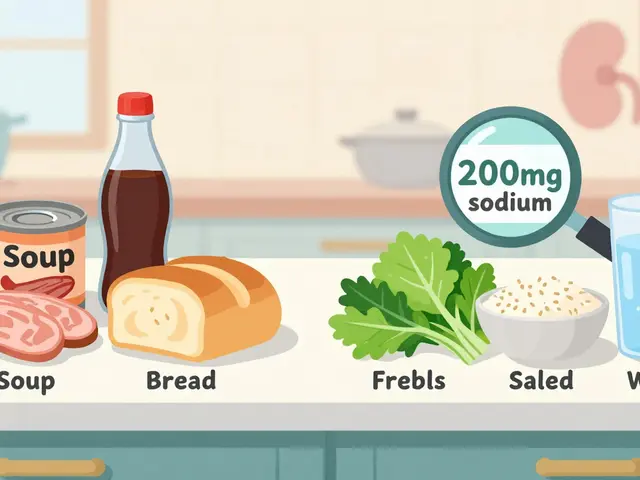
What You Can Do to Lower Your Risk
If your doctor still thinks SGLT2 inhibitors are right for you, don’t panic. There are steps you can take to cut your risk:
- Stay hydrated. Drink plenty of water. It helps flush sugar out of your system faster.
- Practice good hygiene. Wash your genital area daily with mild soap and water. Dry thoroughly. Avoid scented wipes or sprays.
- Don’t hold in urine. Go when you need to. Bacteria thrive when urine sits too long.
- Watch for symptoms. Redness, swelling, pain, or unusual discharge? Fever above 100.4°F? Feeling unwell? Don’t wait. Call your doctor immediately.
- Consider cranberry. A 2023 FDA safety update noted that cranberry products may reduce UTI risk by nearly 30% in SGLT2 users. It’s not a cure, but it’s a simple, low-risk addition.
One study from the Swedish National Diabetes Register found that over 23% of people stopped taking SGLT2 inhibitors within two years because of genital or urinary side effects. That’s more than one in five. If you’re struggling with infections, it’s okay to switch.

What Are the Alternatives?
If infections keep coming back, there are other options that don’t dump sugar into your urine:
- DPP-4 inhibitors (like sitagliptin or linagliptin) lower blood sugar without increasing infection risk. They’re often used when SGLT2 inhibitors aren’t tolerated.
- GLP-1 receptor agonists (like semaglutide or liraglutide) help with weight loss and heart protection-just like SGLT2 inhibitors-but without the urinary side effects.
- Metformin remains the first-line drug for most people. It’s safe, cheap, and doesn’t cause yeast infections.
For someone with heart disease or chronic kidney disease, SGLT2 inhibitors still have a place. But for others, especially those with a history of infections, alternatives are often smarter.
The Bottom Line
SGLT2 inhibitors are powerful tools. They save lives-especially for people with heart failure or kidney disease. But they’re not risk-free. The sugar they flush out doesn’t just vanish. It stays in your body, feeding infections that can turn dangerous fast.
If you’re on one of these drugs and you’re dealing with itching, burning, or recurring UTIs, talk to your doctor. Don’t assume it’s “just a yeast infection.” It might be the start of something worse.
And if you’re considering starting one? Ask: Have I had frequent UTIs before? Am I over 65? Do I have kidney issues? Your answers matter. The right medication for your heart might not be the right one for your bladder.
There’s no one-size-fits-all in diabetes care. Sometimes, the best choice isn’t the newest drug-it’s the one that keeps you healthy, not hospitalized.
Can SGLT2 inhibitors cause yeast infections in men?
Yes. While yeast infections are more commonly reported in women, men taking SGLT2 inhibitors can develop balanitis-an inflammation of the head of the penis. Symptoms include redness, swelling, itching, and discomfort during urination or sex. The cause is the same: excess sugar in the urine creates a breeding ground for Candida fungi. Good hygiene and staying hydrated can help reduce the risk.
How soon after starting SGLT2 inhibitors do infections usually appear?
Most genital yeast infections show up within the first 3 to 6 months of starting the medication. Urinary tract infections can occur anytime, but serious ones like urosepsis often appear around 45 days after beginning treatment, according to FDA data. That’s why it’s critical to monitor symptoms closely during the first few months.
Are SGLT2 inhibitors still safe to use if I’ve had a UTI before?
It depends. If you’ve had occasional, mild UTIs that responded quickly to antibiotics, you may still be a candidate-but you’ll need close monitoring. If you’ve had recurrent, severe, or complicated infections (like kidney infections or sepsis), your doctor will likely recommend switching to a different class of medication, like a GLP-1 agonist or DPP-4 inhibitor, to avoid repeating the problem.
Can drinking more water prevent infections from SGLT2 inhibitors?
Yes, hydration is one of the most effective, low-cost ways to reduce risk. Drinking more water dilutes the sugar in your urine and helps flush out bacteria and yeast before they can multiply. Aim for at least 8 cups (2 liters) daily. Avoid sugary drinks-they’ll make the problem worse. Studies show that people who stay well-hydrated on SGLT2 inhibitors have significantly fewer urinary infections.
Is Fournier’s gangrene a common side effect of SGLT2 inhibitors?
No, it’s rare-but extremely serious. Fournier’s gangrene is a life-threatening necrotizing infection of the genitals and perineum. The European Medicines Agency added a warning about it in 2016 after a small number of cases were reported. It’s estimated to occur in fewer than 1 in 10,000 users. But because it progresses rapidly and can be fatal, you must seek emergency care immediately if you notice sudden pain, swelling, redness, or fever in the genital area.
Do SGLT2 inhibitors cause kidney damage?
They usually protect the kidneys, but not always. In people with healthy kidneys, these drugs slow the progression of kidney disease. But if you develop a severe urinary tract infection that spreads to the kidneys (like pyelonephritis), it can cause acute kidney injury. In rare cases, this leads to permanent damage or the need for dialysis. That’s why treating infections early is so important.
Should I stop taking my SGLT2 inhibitor if I get a yeast infection?
Not necessarily. Mild yeast infections can often be treated with over-the-counter antifungals. But if infections keep coming back, or if you develop fever, back pain, or nausea, contact your doctor right away. You may need to stop the drug temporarily or permanently. Never stop your medication without talking to your healthcare provider-they’ll help you weigh the risks and choose a safer alternative.
If you’re on an SGLT2 inhibitor and feel something’s off-itching, burning, fever, or just a general sense of unease-don’t brush it off. Your body is trying to tell you something. Listen. Talk to your doctor. There are better options out there if the risks outweigh the benefits.







Chris Marel December 8, 2025
I’ve been on dapagliflozin for a year and never had an issue, but my sister got a nasty yeast infection within weeks. I didn’t even know men could get it too-learned that from this post. Glad I’m not the only one noticing how the sugar in urine just… sits there like a buffet for fungi. Weird how something so smart scientifically can have such a dumb side effect.
Arun Kumar Raut December 10, 2025
My uncle in India took one of these pills and ended up in hospital with a kidney infection. He was 70, had high sugar but no heart problems. Doctor said it was the drug. He switched to metformin and never looked back. Why take risks when simple stuff works? We don’t need fancy pills to stay alive. Just clean food, water, and patience.
Carina M December 12, 2025
It is profoundly irresponsible to suggest that cranberry juice is a viable preventative measure for life-threatening urosepsis. The FDA has never endorsed such a claim, and to imply otherwise is not only scientifically indefensible but also dangerously misleading to vulnerable populations. One does not mitigate systemic infection with fruit extract. This is not a salad.
Ajit Kumar Singh December 13, 2025
Bro this is why I dont trust big pharma anymore they sell you a drug that makes you pee sugar and then act surprised when you get infected like what did you think was gonna happen lol they make billions and you pay with your kidneys and your dignity and then they tell you to drink more water like its your fault for not being a perfect human being 🤡
Lisa Whitesel December 15, 2025
The fact that anyone still considers this a viable option for non-cardiac patients is a testament to how badly medicine has been corrupted by marketing. If your HbA1c is above 8.5 you shouldn't be on anything except lifestyle intervention. Period. Stop treating symptoms with side effects and start treating the root cause. This isn't medicine. It's corporate triage.
Raja Herbal December 16, 2025
So let me get this straight… you dump sugar into your bladder, call it ‘science,’ and then tell people to ‘stay hydrated’ like they’re a houseplant? 😂 Meanwhile, your doctor’s got a new BMW from the pharma reps. I’d rather have high sugar than a yeast party in my urethra. Thanks, Big Pharma, for making diabetes feel like a horror movie.
Sarah Gray December 17, 2025
There is a statistically significant correlation between SGLT2 inhibitor use and recurrent genitourinary infections, as evidenced by multiple prospective cohort studies published between 2018 and 2023. The risk-benefit ratio must be evaluated on an individualized basis, with particular attention to anatomical, hormonal, and microbiological variables. To dismiss this as merely ‘bad hygiene’ is both medically inaccurate and culturally dismissive.
Kathy Haverly December 18, 2025
Oh great. So now we’re supposed to be grateful that a drug that turns our urine into a sugar-sweet yeast incubator also ‘protects the heart’? Let me guess-your cardiologist doesn’t have to clean up the sepsis after you’re done bleeding out from a necrotizing infection. Meanwhile, GLP-1 agonists do everything these drugs do… without turning your private parts into a petri dish. Why are we still pretending this is a trade-off and not a scam?
Steve Sullivan December 19, 2025
bro i just took canagliflozin for 3 months and got a yeast thing i thought it was a rash then it was like… wait this is not normal. i went to the doc and they said ‘oh yeah this is normal’ and handed me a cream like it was a coupon 😭 i just wanted to not die from diabetes not become a fungal farm. i switched to metformin and now i feel like a human again. also i love you all. 🤍
George Taylor December 21, 2025
...I just... I don't even know what to say anymore. The fact that this is even a conversation. The fact that we have to weigh ‘heart protection’ against ‘possible necrotizing genital infection.’ The fact that we’re being told to drink water like that’s the solution to a drug-induced sugar bath. I’m not mad. I’m just… disappointed. In everything. 😔