Warfarin to DOAC Switch Timing Calculator
Safe Switch Timing Guide
This tool helps determine when it's safe to switch from warfarin to a direct oral anticoagulant (DOAC) based on your current INR level and the specific DOAC you're switching to.
Why Switch from Warfarin to a DOAC?
Many people on warfarin are switching to a direct oral anticoagulant (DOAC) - and for good reason. Warfarin has been the go-to blood thinner for decades, but it comes with a lot of hassle: frequent blood tests, strict diet rules, and dozens of drug interactions. DOACs like dabigatran, rivaroxaban, apixaban, and edoxaban don’t need regular INR checks, have fewer food interactions, and are just as effective - or even better - at preventing strokes and clots.
But switching isn’t as simple as stopping one pill and starting another. Do it wrong, and you risk a stroke, a dangerous bleed, or both. The key is timing, patient-specific factors, and following proven protocols.
When Is It Safe to Switch?
The biggest danger during the switch is having too little or too much blood thinning. If you stop warfarin too early and start the DOAC too late, your blood can clot. If you start the DOAC too soon, your INR might still be high, and you could bleed.
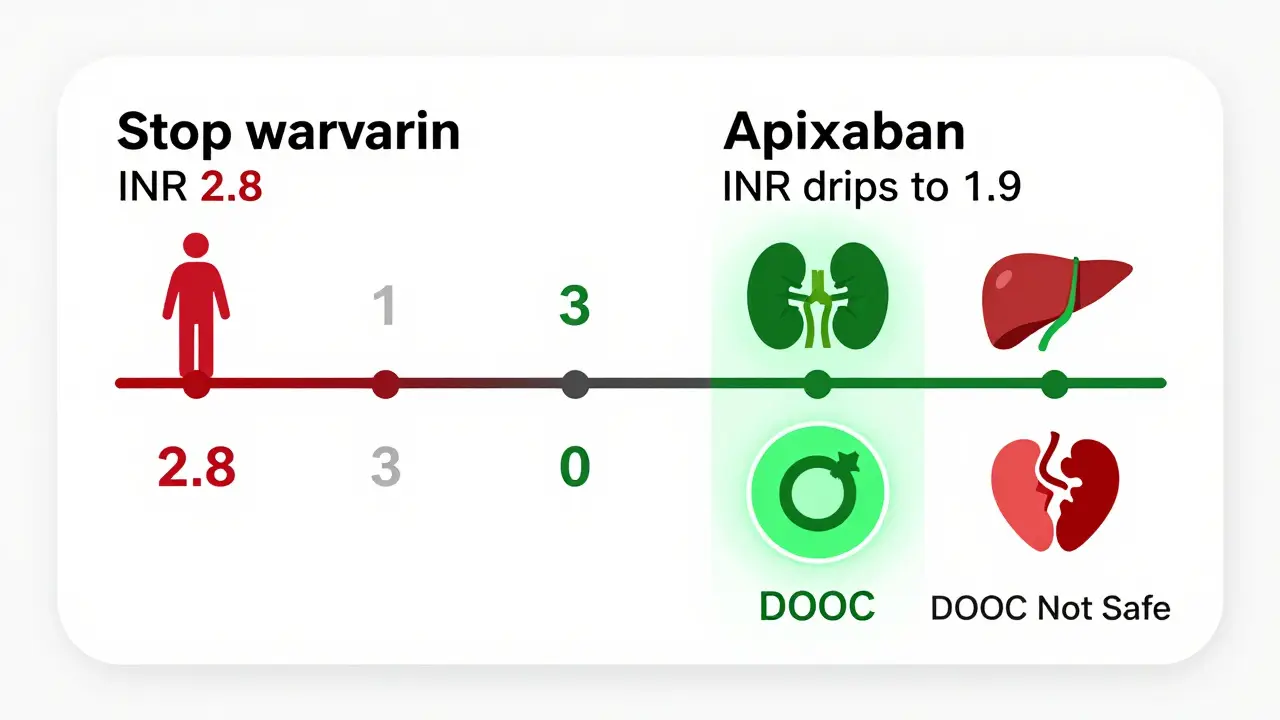
Here’s what the guidelines say about INR levels before starting a DOAC:
- If your INR is ≤2.0: You can start the DOAC right away.
- If your INR is 2.0-2.5: Start the DOAC the same day or wait until the next day.
- If your INR is 2.5-3.0: Wait 1-3 days and recheck your INR.
- If your INR is ≥3.0: Don’t start the DOAC. Wait 3-5 days and retest.
These aren’t guesses - they’re based on clinical trials and real-world outcomes. For example, rivaroxaban can be started when INR is ≤3.0, but apixaban and dabigatran require INR ≤2.0. Edoxaban needs INR ≤2.5. Get this wrong, and you’re playing Russian roulette with your blood.
Who Should NOT Switch?
Not everyone is a candidate for a DOAC. Some people should stay on warfarin - and here’s why.
- Anyone with a mechanical heart valve: DOACs don’t work well here. Warfarin is still the only approved option.
- People with severe kidney problems (CrCl under 15-30 mL/min): Most DOACs are cleared by the kidneys. If your kidneys are failing, the drug builds up and increases bleeding risk.
- Those with advanced liver disease (Child-Pugh Class C): The liver helps metabolize DOACs. If it’s damaged, the drug can stay in your system too long.
- Pregnant or breastfeeding women: DOACs can cross the placenta and harm the baby. Warfarin has risks too, but it’s better understood in pregnancy.
Also, if you weigh less than 60 kg or more than 150 kg, you were mostly left out of the original DOAC trials. That doesn’t mean you can’t switch - but your doctor needs to be extra careful with dosing and monitoring.
What About Bleeding Risks?
DOACs have a better safety profile than warfarin - especially when it comes to brain bleeds. The RE-LY trial showed that dabigatran reduced intracranial hemorrhage by 33% compared to warfarin. That’s huge. Brain bleeds are often deadly, and avoiding them is one of the biggest wins of switching.
But switching periods can be tricky. When you stop warfarin and start a DOAC, there’s a short window where both drugs might be in your system. This overlap can increase the risk of gastrointestinal bleeding - especially if you’re older or have stomach ulcers.
Also, DOACs wear off faster. If you miss a dose, your protection drops in 12-24 hours. That’s why consistency matters. Set phone alarms. Use pill organizers. Don’t skip doses - even if you feel fine.
Special Cases: Kidney Function and Surgery
Your kidneys matter more with DOACs than they did with warfarin. You still need to check your creatinine clearance - not every month, but every 6-12 months if you’re stable.
If you’re scheduled for surgery or a procedure, timing is everything:
- For dabigatran with normal kidney function (CrCl ≥90 mL/min) and a low-risk procedure: Hold it 24-36 hours.
- For the same drug with moderate kidney impairment (CrCl 45 mL/min) and a high-risk surgery: Hold it 96-108 hours (4-4.5 days).
These aren’t random numbers. They’re based on how long it takes the drug to clear from your body. Go too soon, and you bleed. Wait too long, and you clot.
And yes - your doctor should check your kidney function before switching. If you haven’t had a blood test in the last 6 months, don’t switch until you do.
What About Cost and Reversal?
DOACs cost more. In the U.S., a month’s supply can run $500-$700. Warfarin? $10-$30. Insurance often covers DOACs, but you might still pay more out of pocket.
And if you bleed? Reversal agents exist - but only for some DOACs. Idarucizumab reverses dabigatran. Andexanet alfa reverses rivaroxaban, apixaban, and edoxaban. But they’re expensive, hard to get quickly, and not always available in smaller hospitals.
Warfarin can be reversed with vitamin K and fresh frozen plasma - and those are everywhere. That’s still a safety net DOACs don’t fully match.
How to Switch Safely: A Step-by-Step Plan
Here’s what a safe switch looks like in real life:
- Check your last bloodwork: INR, kidney function (CrCl), liver tests - all within the last 6 months.
- Calculate your creatinine clearance using the Cockcroft-Gault equation. Your doctor should do this - don’t guess.
- Check your INR the day before or the day of the switch. Don’t skip this step.
- Based on your INR, follow the timing rules above to decide when to start the DOAC.
- Stop warfarin at the right time. Don’t stop it early just because you’re “ready.”
- Start the DOAC exactly when instructed. No delays. No early starts.
- Get your patient education materials: An anticoagulant alert card, a booklet on atrial fibrillation, and info on what to do if you bleed.
- Follow up with your pharmacist. Many pharmacies offer a New Medicine Service to check in after you start a new blood thinner.
Don’t try to do this on your own. Only clinicians experienced in anticoagulation should manage this switch. That’s not a suggestion - it’s a guideline from the Royal Pharmaceutical Society and the American Heart Association.
What to Watch For After the Switch
Once you’re on a DOAC, you’re not out of the woods. Here’s what to watch:
- Bleeding: Unusual bruising, nosebleeds that won’t stop, blood in urine or stool, vomiting blood, or severe headaches (could mean brain bleed).
- Missed doses: If you forget a pill, take it as soon as you remember - but only if it’s within 6 hours. If it’s been longer, skip it. Never double up.
- Drug interactions: Some antibiotics, antifungals, and seizure meds can raise DOAC levels. Always tell your doctor or pharmacist about every new medicine - even over-the-counter ones.
- Storage: Dabigatran is moisture-sensitive. Keep it in the original bottle. Other DOACs can go in pill boxes - but not dabigatran.
And remember: DOACs don’t show up on standard blood tests. If you ever need emergency care, make sure the ER team knows you’re on a DOAC. Carry your alert card.
Final Thoughts: Is Switching Right for You?
For most people with non-valvular atrial fibrillation, deep vein thrombosis, or pulmonary embolism, switching from warfarin to a DOAC is a win. Fewer blood tests. Fewer dietary restrictions. Lower risk of brain bleeds.
But it’s not for everyone. If you have a mechanical valve, bad kidneys, or liver disease, stay on warfarin. If you’re pregnant or can’t afford the cost, talk to your doctor about options.
The switch works best when it’s planned, measured, and supervised. Don’t let convenience override safety. A few extra blood tests now can prevent a stroke - or a bleed - later.
Can I switch from warfarin to a DOAC on my own?
No. Switching from warfarin to a DOAC requires precise timing based on your INR level, kidney function, and medical history. Only clinicians trained in anticoagulation management should make this change. Doing it without proper guidance increases your risk of stroke or serious bleeding.
Do I still need blood tests after switching to a DOAC?
You won’t need regular INR tests anymore - that’s one of the main benefits. But you still need kidney function tests (creatinine and eGFR) every 6-12 months. DOACs are cleared by the kidneys, and if your kidney function drops, your drug levels can rise dangerously.
What if I miss a dose of my DOAC?
If you miss a dose and remember within 6 hours, take it right away. If it’s been longer than 6 hours, skip the missed dose and take your next one at the regular time. Never double up. DOACs wear off quickly - missing a dose means your protection drops in 12-24 hours, so consistency is critical.
Are DOACs safer than warfarin for older adults?
Yes - for most older adults. DOACs reduce the risk of brain bleeds, which are more common and deadly in older people. They also don’t require frequent blood tests, which can be hard to manage with mobility or cognitive issues. But kidney function must be checked regularly, and dosing may need to be adjusted for lower body weight or frailty.
Can I take other medications while on a DOAC?
Some medications can interfere with DOACs. Common culprits include certain antibiotics (like clarithromycin), antifungals (like ketoconazole), seizure drugs (like carbamazepine), and even some herbal supplements like St. John’s wort. Always check with your pharmacist before starting any new medicine - even aspirin or ibuprofen.
What if I need emergency surgery?
If you need emergency surgery, tell the medical team you’re on a DOAC. Bring your anticoagulant alert card. For some DOACs, reversal agents exist - like idarucizumab for dabigatran or andexanet alfa for factor Xa inhibitors - but they’re not always immediately available. The team will decide whether to proceed based on your last dose timing and kidney function.







Elen Pihlap January 7, 2026
i switched last year and honestly? my life changed. no more weekly blood draws. no more eating salad every damn day. i forgot what it was like to not worry about broccoli ruining my meds. i still get nervous when i miss a dose though 😅
Sai Ganesh January 7, 2026
In India, access to DOACs is still a challenge. Many patients are stuck with warfarin due to cost, even if it’s less convenient. We need better healthcare policies to make these life-saving drugs affordable for everyone.
Paul Mason January 9, 2026
Look, if you’re thinking of switching, just do it. But only if your INR is under 2.0 and your kidneys are okay. I’ve seen too many people skip the blood tests and end up in the ER. Don’t be that guy. Your doctor isn’t being extra - they’re keeping you alive.
Katrina Morris January 9, 2026
i started apixaban last month and its been so much easier no more warfarin stress but i forgot to tell my dentist and they almost did a procedure without holding it 😳 i carry my card now
steve rumsford January 10, 2026
my grandma switched to dabigatran and now she uses a pill box with alarms and still forgets half the time. she almost bled out after a fall because she didn’t tell the ER she was on it. if you’re on one of these, tell EVERYONE. your life depends on it.
Andrew N January 12, 2026
The article mentions reversal agents but doesn’t emphasize how rare they are outside major hospitals. Andexanet costs $30k per dose. Most ERs don’t stock it. If you bleed, you’re basically praying. Warfarin’s reversal is cheap and everywhere. DOACs aren’t magic - they’re expensive gamble.
LALITA KUDIYA January 13, 2026
my mom is on rivaroxaban and she loves it but she also takes turmeric for arthritis and i told her to stop it. even natural stuff can mess with these drugs. just be careful out there 🙏
Poppy Newman January 13, 2026
Just switched to apixaban last week 🎉 No more INR checks = pure joy. But I did cry when I saw the bill. $680/month 😭 Insurance covered 80% but still… I’m so grateful I can afford it. For those struggling - talk to your pharma rep. They have patient programs.
Anthony Capunong January 14, 2026
I don’t trust these newfangled pills. Back in my day, we took warfarin and we liked it. You want to live long? Stick to what’s been proven. These DOACs are just Big Pharma’s money grab. And now we’re paying for it.
Aparna karwande January 16, 2026
People think switching is easy because it’s trendy. But in India, most doctors don’t even know the correct timing for DOACs. I saw a patient start edoxaban with INR 3.2. That’s not negligence - that’s criminal. Someone needs to be held accountable.
Jessie Ann Lambrecht January 18, 2026
I’m a nurse and I’ve helped over 50 patients switch. The biggest win? Less brain bleeds. The biggest win? People actually take their meds because it’s simpler. Yes, it’s expensive. Yes, reversal is harder. But for most of us? It’s worth it. Talk to your pharmacist - they’re your secret weapon.
Vince Nairn January 18, 2026
So you’re telling me I can’t just stop warfarin on a Friday and start a DOAC on Monday because I’m ‘done with this nonsense’? Wow. What a shocker. Guess I’ll just keep bleeding quietly and pretending I’m fine.