Acid Suppression: Understanding Medications, Risks, and Alternatives
When you hear acid suppression, the use of medications to reduce stomach acid production. Also known as gastric acid reduction, it's one of the most common treatments for heartburn, GERD, and ulcers. But here’s the thing: popping a pill every day isn’t harmless. These drugs change how your body digests food, absorbs nutrients, and even fights off infections.
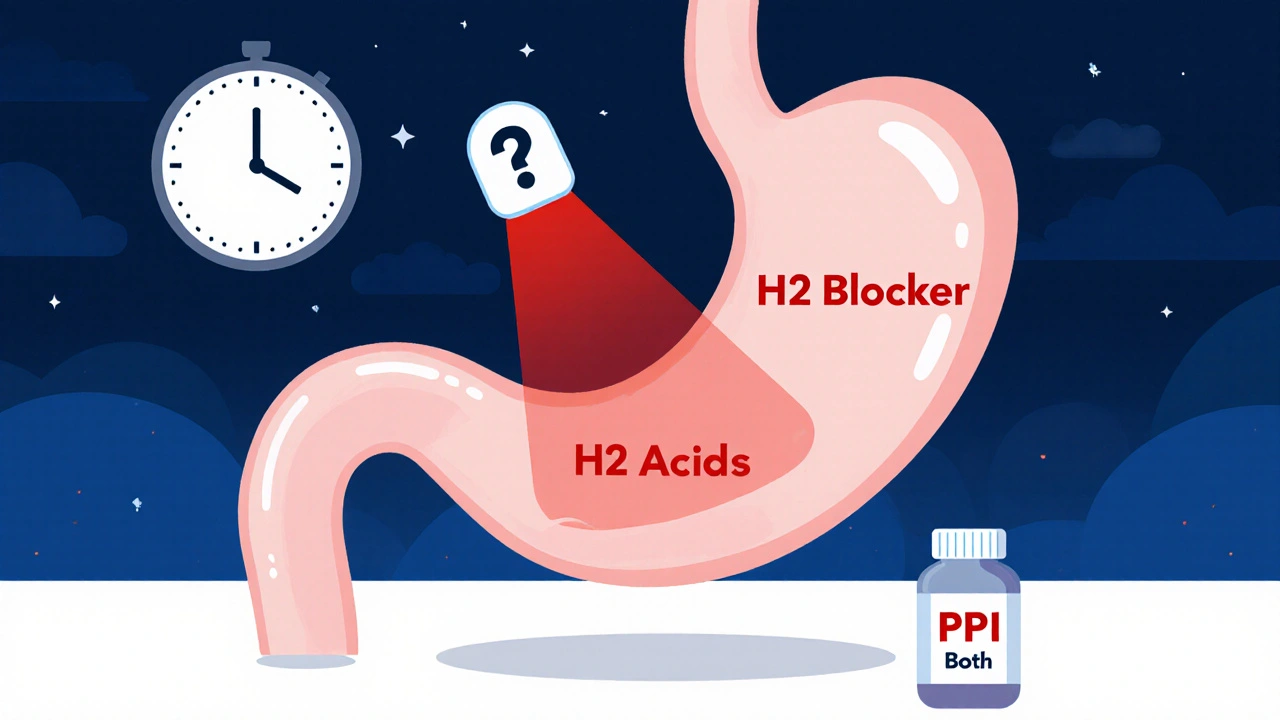
Proton pump inhibitors, a class of drugs that block acid production at its source. Also known as PPIs, they include omeprazole, esomeprazole, and lansoprazole. They work great—fast and strong. But studies show long-term use links to lower magnesium, vitamin B12 deficiency, and even a higher chance of kidney problems. Then there’s H2 blockers, medications like famotidine and ranitidine that reduce acid by targeting histamine receptors. Also known as histamine-2 receptor antagonists, they’re milder and often used for short-term relief. They don’t shut down acid completely, which might be safer for some people. But neither type fixes the root cause—whether it’s a hiatal hernia, obesity, or eating too close to bedtime.
People often stay on acid suppressors for years because symptoms disappear. But the body adapts. When you stop, acid can come back harder. That’s rebound hyperacidity. And it’s not just about discomfort—it’s about your gut lining, your microbiome, and how well you absorb calcium, iron, and other essentials. Some folks find relief with simple changes: smaller meals, avoiding spicy or fatty foods, elevating the head of the bed, or losing weight. Others need a different kind of help—like treating H. pylori infection or adjusting medications that irritate the stomach.
What you’ll find below are real, no-fluff guides on how acid suppression connects to other health issues. From how PPIs interfere with kidney function and nutrient absorption, to why some people end up with dangerous side effects from long-term use. You’ll see how acid suppression ties into opioid constipation, fiber supplements blocking meds, and even how liver health plays into detox and medication safety. These aren’t random posts—they’re the exact conversations people are having when they realize their daily pill isn’t the whole answer.
H2 Blockers and PPIs: When Combining Acid Reducers Does More Harm Than Good
Combining H2 blockers and PPIs is common but often unnecessary. Learn why this practice increases risks without improving outcomes-and what to do instead.