Benzoyl Peroxide Pregnancy Safety Quiz
1. What is the FDA pregnancy category for benzoyl peroxide?
2. Which factor most increases percutaneous absorption of benzoyl peroxide?
3. According to the AAD, what is the recommended starting concentration for pregnant patients?
Benzoyl Peroxide is a topical oxidizing agent commonly used to treat acne, available in concentrations from 2% to 10% and prized for its antibacterial and keratolytic properties. Expecting mothers often wonder if that familiar over‑the‑counter spot treatment is safe for the developing baby. This article breaks down the science, regulatory stance, and practical advice so you can decide with confidence.
Quick Takeaways
- Current research shows minimal systemic absorption of benzoyl peroxide, making it low‑risk for most pregnancies.
- The U.S. FDA classifies it as a Category C drug, meaning animal studies show some risk but human data are insufficient.
- Dermatologists typically recommend limiting use to small areas, avoiding broken skin, and opting for lower concentrations (2‑5%).
- Safer alternatives such as Azelaic Acid or Salicylic Acid at low doses can be considered when caution is needed.
- Always consult your Dermatologist before starting any acne regimen during pregnancy.
How Benzoyl Peroxide Works on the Skin
When applied, benzoyl peroxide releases oxygen, creating an environment hostile to Propionibacterium acnes (the bacteria that fuels acne). It also softens keratin plugs, helping clogged pores clear. The oxidation reaction is largely confined to the skin’s surface, with less than 0.01% of the dose entering the bloodstream-a key factor when assessing fetal exposure.
Pregnancy‑Related Skin Changes and Acne
Hormonal shifts in Pregnancy increase sebum production, often worsening acne in the second and third trimesters. Many women experience “pregnancy‑related acne” and seek fast‑acting treatments. Understanding the balance between effective skin control and fetal safety becomes critical.
Regulatory Perspective: FDA and Teratogenicity
The U.S. Food and Drug Administration (FDA) places benzoyl peroxide in Pregnancy Category C. Category C indicates that animal studies have shown some adverse effects, but well‑controlled studies in pregnant women are lacking. Importantly, the FDA notes the lack of evidence for teratogenicity (birth defects) in humans because systemic exposure is negligible.
Internationally, the European Medicines Agency (EMA) mirrors this stance, labeling the ingredient as “use with caution.” Both agencies advise physicians to weigh the benefits against potential risks, especially when alternative treatments exist.

Key Pharmacokinetic Factors: Percutaneous Absorption
Three pharmacokinetic parameters dictate safety:
- Percutaneous absorption rate: Studies using radiolabeled benzoyl peroxide show less than 0.02% penetration through intact skin.
- Concentration: Higher percentages (8‑10%) increase local irritation and marginally raise systemic levels.
- Skin integrity: Broken or inflamed skin can boost absorption, which is why dermatologists advise against applying the product on open wounds.
Clinical Guidance from Dermatology Boards
The American Academy of Dermatology (AAD) recommends the following for pregnant patients:
- Start with the lowest effective concentration (2% or 2.5%).
- Apply once daily, preferably in the evening to reduce oxidation‑induced dryness.
- Limit treatment to affected areas (e.g., forehead, chin) and avoid the perioral region.
- Monitor for excessive redness or peeling; if observed, discontinue and switch to a gentler option.
When severe nodular acne threatens scarring, a dermatologist may still prescribe benzoyl peroxide, citing its low systemic exposure compared with oral antibiotics or isotretinoin, which are contraindicated.
Safer Alternatives for Expecting Mothers
If you prefer to err on the side of caution, consider these options, each with documented pregnancy safety profiles:
| Agent | FDA Category | Typical Concentration | Absorption Rate | Notes |
|---|---|---|---|---|
| Benzoyl Peroxide | Category C | 2‑5% | <0.02% | Effective, low systemic exposure |
| Azelaic Acid | Category B | 15‑20% | ~0.01% | Anti‑inflammatory, safe for melasma |
| Salicylic Acid | Category C (≤2%) | 0.5‑2% | <0.01% | Avoid high concentrations; can cause fetal toxicity |
| Sulfur | Category B | 5‑10% | ~0.02% | Mild, may cause odor |
These alternatives are especially useful for women with sensitive skin or who experience irritation from benzoyl peroxide.
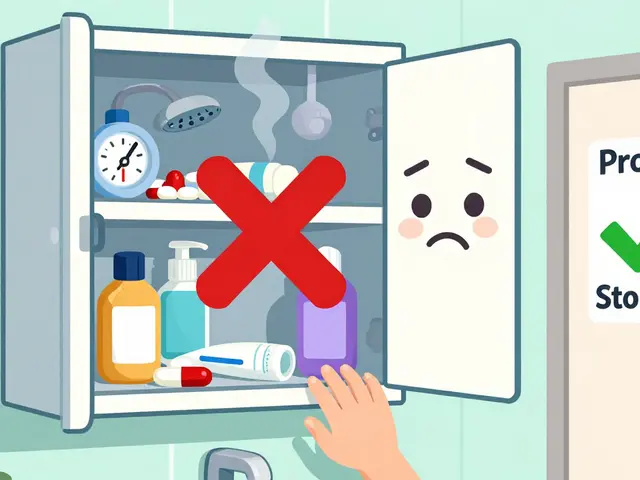
Practical Tips for Using Benzoyl Peroxide Safely
- Patch test first: Apply a pea‑sized amount on the inner forearm for 24hours to gauge tolerance.
- Moisturize: Pair the treatment with a fragrance‑free, non‑comedogenic moisturizer to reduce dryness.
- Sun protection: Benzoyl peroxide can increase photosensitivity; use a broad‑spectrum SPF30+.
- Avoid oral ingestion: Though unlikely, keep the product away from the mouth and wash hands thoroughly after application.
- Monitor pregnancy milestones: Discuss any skin changes with your obstetrician during routine prenatal visits.
When to Stop Using Benzoyl Peroxide
If any of the following occur, discontinue use and seek professional advice:
- Severe erythema, swelling, or blistering.
- Signs of systemic reaction such as dizziness or nausea.
- Development of new skin conditions (e.g., rash unrelated to acne).
In most cases, these reactions stem from over‑use or application on compromised skin rather than inherent toxicity.

Frequently Asked Questions
Is benzoyl peroxide safe to use during the first trimester?
The first trimester is a critical period for organ development, but studies show that topical benzoyl peroxide has minimal systemic absorption. Most dermatologists advise using the lowest effective concentration (2%) and limiting application to small areas. If you have concerns, discuss alternative options with your doctor.
Can benzoyl peroxide cause birth defects?
Current human data do not link topical benzoyl peroxide to congenital anomalies. Animal studies have shown some toxicity at high systemic doses, which is why the FDA assigns Category C. Because the drug stays largely on the skin, the risk of birth defects is considered very low.
Should I switch to azelaic acid instead?
Azelaic acid is a Category B ingredient, meaning animal studies show no risk and there’s limited human data. It’s a good alternative for those who experience irritation from benzoyl peroxide or prefer a gentler anti‑inflammatory action. However, it may work slower for severe acne.
How long should I wait after stopping benzoyl peroxide before delivering?
Because the drug clears from the skin within 24‑48hours, there’s no required wash‑out period before delivery. You can stop use anytime you feel uncomfortable, and the skin will return to its baseline state shortly after.
Is it okay to use benzoyl peroxide while breastfeeding?
Breast milk exposure is considered negligible due to the same low systemic absorption seen in pregnancy. Most lactation consultants deem it acceptable, especially at low concentrations, but a brief patch test is advisable to ensure no irritation for the mother.






Hardy D6000 September 23, 2025
The article glosses over the fact that benzoyl peroxide, while marketed as a benign over‑the‑counter remedy, is fundamentally an oxidizing agent capable of generating free radicals at the site of application; such radicals, though ostensibly confined to the epidermis, can induce systemic oxidative stress when used repeatedly over large surface areas. Moreover, the FDA’s Category C designation is not a mere bureaucratic footnote but a clear signal that animal studies have demonstrated teratogenic potential, even if human data remain scant. The claim that less than 0.01% of the dose enters the bloodstream does not account for cumulative exposure over a trimester, especially when pregnant individuals may apply the product daily without medical supervision. It is also noteworthy that the cited percutaneous absorption figures derive primarily from studies on intact skin, yet the article itself admits that broken or inflamed skin dramatically increases absorption-a condition not uncommon among acne‑prone expectant mothers. Consequently, the recommendation to “limit use to small areas” is an oversimplification that fails to consider the variability in lesion distribution and patient compliance. While the AAD’s guidance on low concentrations seems reasonable, it remains an opinion rather than an evidence‑based protocol, and the lack of large‑scale, controlled trials in pregnant populations should temper any blanket endorsement. In practice, physicians often prioritize non‑oxidative alternatives precisely because the risk–benefit calculus for benzoyl peroxide is, at best, equivocal. Finally, the article’s brief mention of alternatives like azelaic acid neglects the fact that even these agents have nuanced safety profiles that warrant individualized assessment. In summary, the ostensibly reassuring tone of the guide masks a series of unresolved pharmacological uncertainties that merit a more cautious, perhaps even skeptical, approach.
Amelia Liani September 23, 2025
Reading this, my heart goes out to all the soon‑to‑be moms out there juggling skin woes and baby worries. Your breakdown is crystal‑clear, and I love how you’ve highlighted both the science and the practical steps. The reminder to keep it low‑dose and steer clear of broken skin feels especially kind. It’s comforting to know there are gentler options like azelaic acid when you need a safer route. Thank you for weaving empathy into the facts-so many posts feel cold and clinical, but yours feels like a supportive hand.
shikha chandel September 23, 2025
One must question the hidden agendas that pervade dermatological literature. The “Category C” label is a veil for corporate complacency. Trust not the surface narrative.
Zach Westfall September 23, 2025
Here’s the thing man benzoyl peroxide is like fireworks for your pores it’s dramatic but it can burn you if you ain’t careful it’s not just a teen‑phase product it stays in the market for a reason use it sparingly and watch for irritation
Pranesh Kuppusamy September 23, 2025
While the enthusiasm of my predecessor is understandable, it is imperative to contextualize the oxidative cascade within a broader existential framework. The very act of applying a peroxide compound to a pregnant epidermis invokes a silent dialogue with unseen biochemical forces that may be hijacked by obscure surveillance mechanisms embedded within pharmaceutical supply chains. Moreover, the purported safety of low‑dose regimens rests upon data selectively curated by entities vested in commercial continuity. Hence, a judicious practitioner must weigh not only dermal outcomes but also the epistemic integrity of the studies cited. In this light, a return to primordial, plant‑based remedies may offer a philosophically coherent alternative.
Crystal McLellan September 23, 2025
lol they hide the truth in plain sight