Arrhythmia Treatment: Medications, Risks, and What Actually Works
When your heart beats too fast, too slow, or irregularly, you’re dealing with an arrhythmia, a condition where the electrical signals that coordinate heartbeats don’t work properly. Also known as heart rhythm disorder, it can feel like fluttering, skipped beats, or a pounding chest—and in some cases, it’s life-threatening. Arrhythmia isn’t one disease. It includes atrial fibrillation, a common type where the upper chambers of the heart quiver instead of beating normally, ventricular tachycardia, a rapid heartbeat starting in the lower chambers that can lead to sudden cardiac arrest, and many others. The right treatment depends on what kind you have, how severe it is, and whether other conditions like heart failure or high blood pressure are involved.
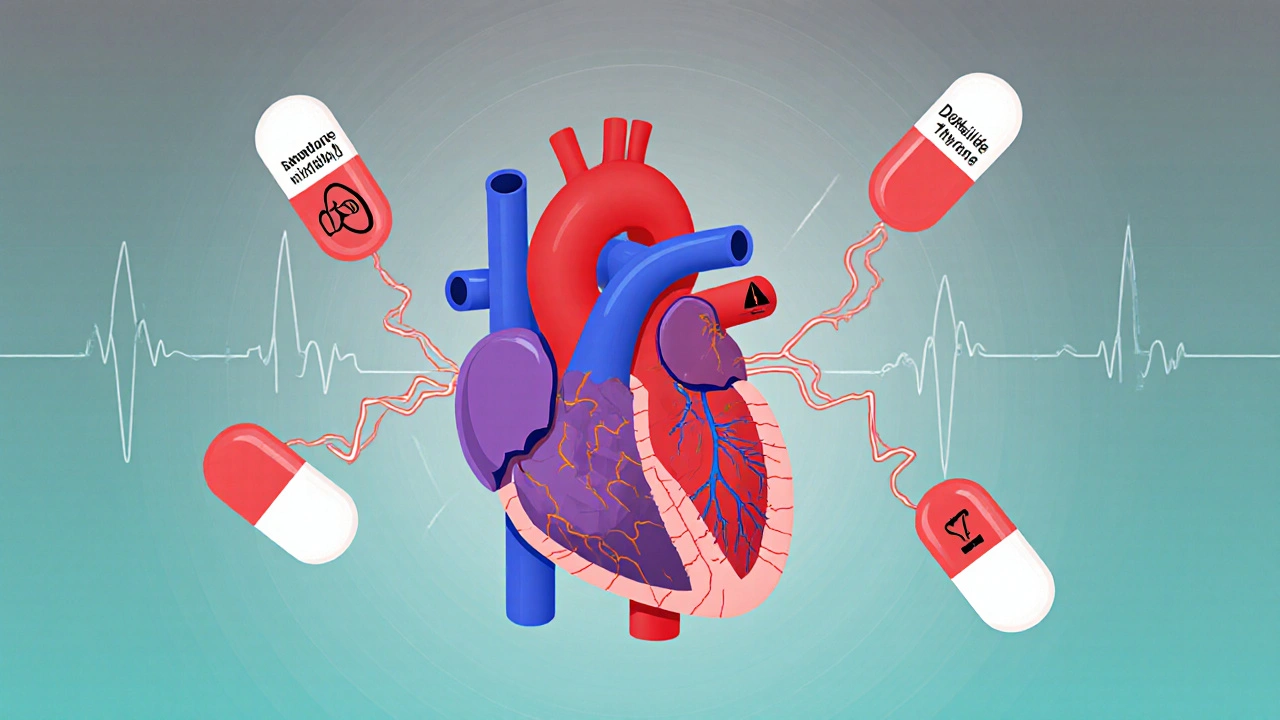
Most people start with antiarrhythmic drugs, medications designed to restore normal heart rhythm by affecting the heart’s electrical activity. These include beta-blockers like metoprolol, calcium channel blockers like diltiazem, and drugs like amiodarone or flecainide. But these aren’t harmless. Many carry black box warnings, the FDA’s strongest alerts for drugs that can cause serious or fatal side effects. For example, some antiarrhythmics can trigger worse arrhythmias instead of fixing them. That’s why doctors don’t just pick a drug off a list—they monitor closely, often using ECGs and blood tests. You also can’t ignore lifestyle factors. Alcohol withdrawal, for instance, can cause dangerous heart rhythms, and some people with arrhythmia are told to avoid stimulants like caffeine or decongestants that raise blood pressure. Even something as simple as a fiber supplement can interfere with how your heart meds are absorbed if taken at the wrong time.
There’s no one-size-fits-all fix. Some people need a pacemaker. Others require ablation. A few might even need surgery. But for most, managing arrhythmia means understanding your triggers, taking meds exactly as prescribed, and knowing when to call 911. Chest pain, dizziness, or passing out aren’t just inconvenient—they can be warning signs. Below, you’ll find real, practical guides on the drugs used, the risks you might not know about, and how other conditions like kidney health or liver damage can change your treatment plan. No fluff. Just what you need to stay safe and informed.
Compare Cordarone (Amiodarone) with Alternatives: What Works Best for Arrhythmias
Cordarone (Amiodarone) is a powerful but risky heart rhythm drug. Learn how it compares to safer alternatives like sotalol, dofetilide, and dronedarone - and when each option makes sense.