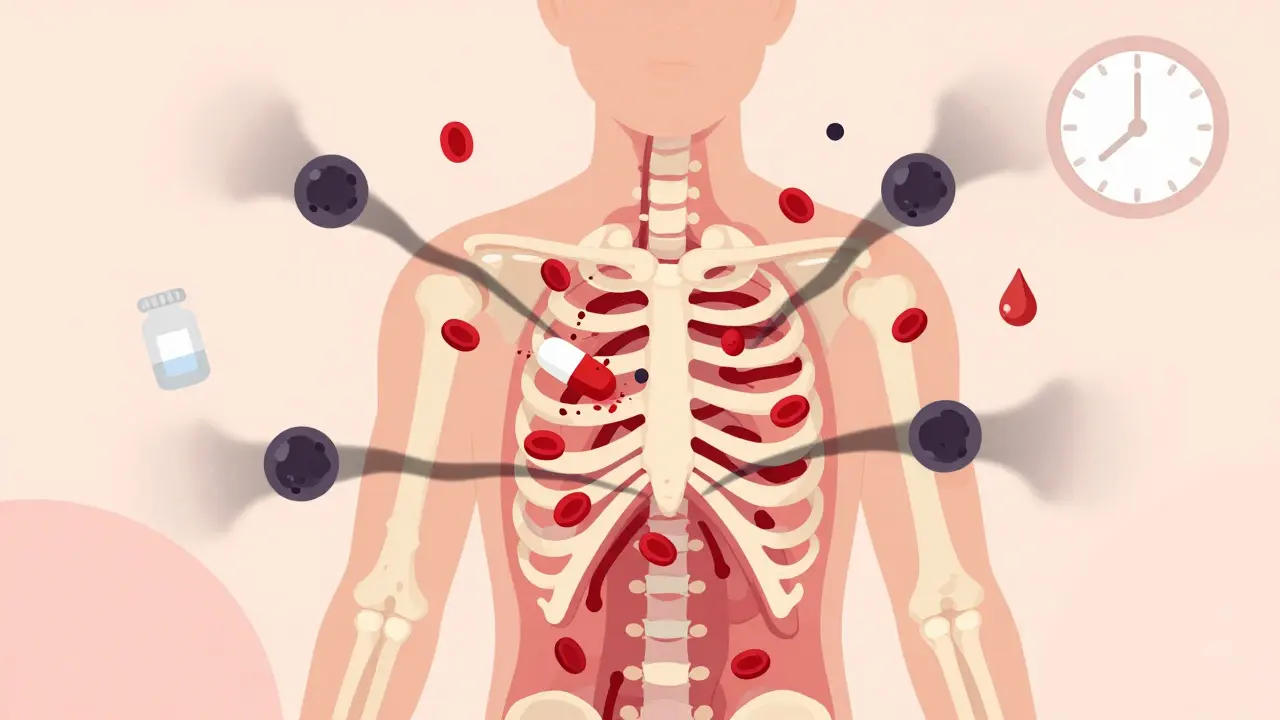
Most people don’t think about their meds doing more than helping them feel better. But some drugs can quietly shut down your bone marrow - the factory inside your bones that makes all your blood cells. When this happens, it’s called medication-induced aplastic anemia. It’s rare, but when it strikes, it moves fast. And if you don’t catch it early, it can turn deadly.
What Exactly Is Medication-Induced Aplastic Anemia?
Your bone marrow doesn’t just make red blood cells - it makes white blood cells to fight infection and platelets to stop bleeding. When a drug damages the stem cells that do this job, your body can’t replace them. The result? A dangerous drop in all three types of blood cells. This isn’t just low iron or a mild side effect. This is your blood production system failing.
It’s not caused by every medication. But certain ones carry real risk. Chloramphenicol, an old antibiotic, is the most notorious - one in every 24,000 to 40,000 people who take it develop this condition. Carbamazepine and phenytoin, used for seizures, increase risk by about 15 times. Even common drugs like NSAIDs (ibuprofen, naproxen), sulfonamide antibiotics, and gold injections for arthritis have been linked. Chemotherapy can cause temporary bone marrow suppression, but true aplastic anemia - where the marrow doesn’t recover - happens in 1-2% of cases.
What makes this different from other side effects? It’s not dose-dependent in most cases. You don’t have to take a lot for it to happen. It’s often an unpredictable immune reaction or direct toxicity that kills your stem cells. And once it starts, it doesn’t pause - it keeps getting worse.
Early Signs You Can’t Afford to Ignore
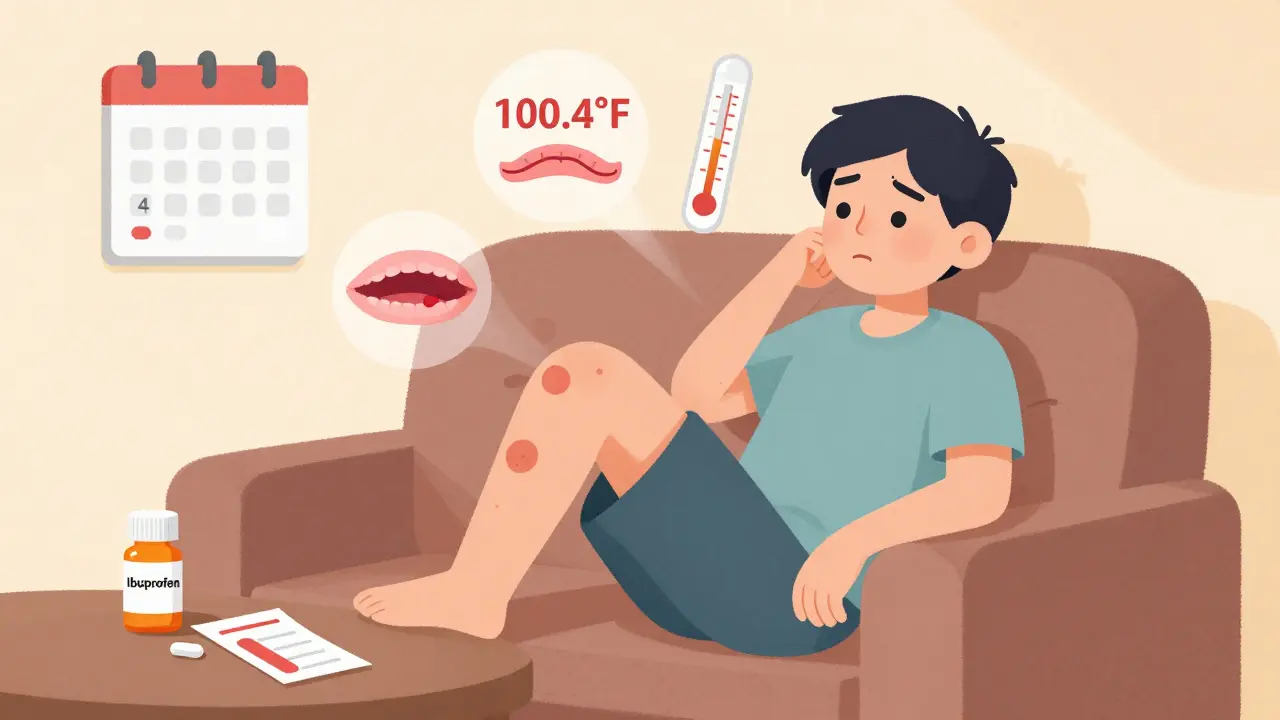
The worst part? The first signs are easy to brush off. You’re tired. You’ve been stressed. You had a cold last week. But if these symptoms stick around - and pile up - it’s not normal.
- Unrelenting fatigue: Not just tired after work. Exhausted even after a full night’s sleep. This isn’t burnout - it’s your body starving for oxygen because your red blood cells are vanishing.
- Unexplained bruising: Purple marks on your legs without bumping into anything. Multiple bruises appearing at once? That’s your platelets dropping. You can’t clot properly anymore.
- Recurrent fevers: Low-grade, persistent fevers between 99°F and 101°F. No infection you can name. Just a fever that won’t quit. This means your white blood cells are gone - your body can’t fight off even tiny invaders.
- Easy bleeding: Nosebleeds that won’t stop, bleeding gums when you brush your teeth, or heavy periods when they’ve always been normal.
- Weight loss without trying: Losing 5-10 pounds in 2-3 weeks with no change in diet or exercise.
These symptoms don’t show up overnight. They creep in over 4-6 weeks. In fact, 68% of patients in one survey didn’t realize something was wrong until they’d been feeling off for over a month. And here’s the scary part: your blood counts drop before you even feel symptoms. By the time you’re exhausted and bruising, your bone marrow is already in crisis.
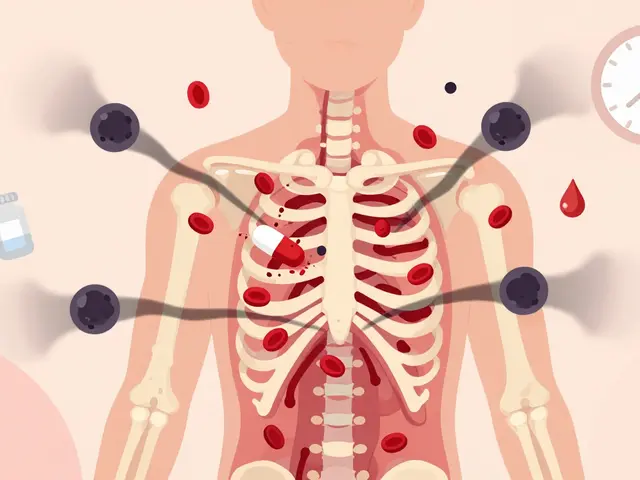
Why Delaying Diagnosis Is Dangerous
Every day matters. If you wait too long, the numbers don’t just get low - they crash.
Here’s what doctors look for in a blood test:
- Hemoglobin under 10 g/dL
- Neutrophils (infection fighters) under 1,500/μL
- Platelets under 150,000/μL
But if you’re in the severe range - neutrophils under 500/μL, platelets under 20,000/μL, or reticulocytes under 40,000/μL - you’re in emergency territory. About 70% of medication-induced cases are already severe by the time they’re diagnosed.
And here’s the hard truth: survival rates drop fast. If you’re diagnosed and treated within two weeks of symptoms starting, your chance of living five years is over 90%. Wait eight weeks? That number plummets to 55%. The difference isn’t just medical - it’s life or death.
Why do people wait? Because doctors miss it. In one study, 72% of patients were first told they had a virus or stress. Pharmacists were sometimes the first to suspect the problem - not the doctor. Patients who kept a full list of their meds - including over-the-counter drugs and supplements - got diagnosed 6.2 days faster on average. That’s critical time.
What to Do Right Now - The Urgent Actions
If you’re on one of these high-risk meds and you’re feeling off - stop the drug. Immediately. Not tomorrow. Not after your next appointment. Now.
Then call your doctor or go to urgent care. Say: “I’m on [drug name], and I’m having symptoms of possible bone marrow failure. I need a CBC right away.” Don’t wait for a referral. Don’t hope it goes away. Push for a complete blood count within 24 hours.
If your platelets are under 50,000/μL, you need to see a hematologist within 48 hours. If they’re under 10,000/μL or you’re actively bleeding, you need a transfusion - and fast.
If your neutrophils drop below 500/μL, you’re at extreme risk for deadly infections. You’ll need to be hospitalized. Antibiotics will start immediately. You’ll be put in reverse isolation - no visitors with colds, no fresh flowers, no raw food. This isn’t overcaution - it’s survival.
And if you develop a fever above 100.4°F (38°C)? Go to the ER. Now. Don’t call your doctor. Don’t wait to see if it breaks. Fever with low blood counts is a medical emergency. You have one hour to get help.
What Happens After Stopping the Drug?
Stopping the medication is step one - but it’s not always enough. In mild cases, your marrow might recover on its own within 4-8 weeks. But in severe cases, you’ll need more.
Doctors now use immunosuppressive therapy - drugs like horse anti-thymocyte globulin and cyclosporine - to calm the immune system’s attack on your stem cells. This works in 78% of cases, according to recent European data. For younger patients with a matched donor, a bone marrow transplant is still the gold standard, with survival rates over 90%.
But here’s the warning: never restart the drug that caused it. Even if you recovered, restarting it carries a 90% chance of a much worse relapse. That’s not a risk worth taking.

Who Should Be Extra Careful?
If you’re starting one of these drugs - chloramphenicol, carbamazepine, phenytoin, gold salts, or certain NSAIDs - ask your doctor about baseline blood work. Get a CBC before you start. Then get tested again after two weeks and again after four.
Some clinics now use electronic alerts in their systems to flag high-risk prescriptions. But not all do. If your doctor doesn’t mention monitoring, ask. Especially if you’re over 60, have a history of autoimmune disease, or are on multiple medications.
And if you’re a parent? Kids can get this too. Symptoms in children are often mistaken for growing pains or viral illnesses. If your child has unexplained fatigue, bruising, or fevers for more than a week - get blood work.
What’s Changing in 2026?
There’s new hope. A NIH clinical trial using a genetic blood test can now spot medication-induced bone marrow failure within 48 hours - with 92% accuracy. That’s a game-changer. The AAMDS Foundation also launched a free mobile app that lets you log symptoms and blood counts. Users saw a 40% drop in diagnostic delays.
Regulators are catching up, too. The European Medicines Agency now requires stronger warnings on carbamazepine labels. The FDA is pushing drug makers to test for bone marrow toxicity earlier in development.
But the biggest change? Awareness. More doctors are learning to recognize the early signs. More patients are speaking up. And that’s what saves lives.
Final Takeaway: Know Your Meds, Know Your Body
You don’t need to fear every pill you take. But you do need to respect the ones that carry risk. If you’re on one of them, keep a list. Track how you feel. Don’t ignore fatigue, bruising, or fevers. If something feels off for more than a week - get a CBC. Don’t wait. Don’t hope. Act.
Medication-induced aplastic anemia is rare. But it’s preventable - if you catch it early. And early detection? That’s not just good medicine. It’s your best shot at staying alive.
Can over-the-counter drugs like ibuprofen cause aplastic anemia?
Yes. While rare, NSAIDs like ibuprofen, naproxen, and aspirin have been linked to medication-induced aplastic anemia. The risk is much lower than with drugs like chloramphenicol or carbamazepine, but it’s real. If you’re taking these daily for months and start experiencing unexplained fatigue, bruising, or fevers, get a blood test. Don’t assume it’s just a side effect.
How long does it take for symptoms to appear after starting a risky medication?
Symptoms usually appear between 2 and 8 weeks after starting the drug. In some cases, they can show up as early as 10 days. The blood counts often drop before you feel sick - so lab tests are key. That’s why doctors recommend a baseline CBC before starting high-risk drugs, followed by weekly checks for the first month.
Is aplastic anemia from meds reversible?
It can be - if caught early. Stopping the drug immediately gives your bone marrow a chance to recover. In mild cases, blood counts bounce back in 4-8 weeks. In severe cases, you’ll need immunosuppressive therapy or a transplant. But if you delay treatment, the damage can become permanent. Recovery isn’t guaranteed - but speed is your biggest ally.
Can you get aplastic anemia from antibiotics like penicillin?
Yes. Sulfonamide antibiotics (like Bactrim) and some penicillin derivatives have been tied to aplastic anemia. It’s not common, but it’s well-documented. The mechanism is often immune-related - your body mistakenly attacks your own bone marrow. If you’re on one of these and develop unexplained bruising or fevers, stop the drug and get tested immediately.
What should I do if I think I have medication-induced aplastic anemia?
Stop the suspected medication immediately. Call your doctor or go to urgent care. Demand a complete blood count (CBC) within 24 hours. If your platelets are under 50,000 or neutrophils under 1,500, ask for a referral to a hematologist. If you have a fever above 100.4°F, go to the ER right away - don’t wait. Keep a full list of all medications you’ve taken in the last 6 months. That information saves lives.





Alexandra Enns January 25, 2026
Okay but let’s be real - if you’re taking ibuprofen daily and not getting a CBC every month, you’re basically playing Russian roulette with your bone marrow. I’ve seen this happen to a friend in Toronto - they thought it was ‘just fatigue’ until their platelets hit 8K. Now they’re on immunosuppressants and can’t even hug their grandkids without a mask. The system is broken. Pharma doesn’t warn you because they don’t have to. Wake up, people.
Marie-Pier D. January 27, 2026
I’m so glad someone finally put this out there 💔 My sister was misdiagnosed for 6 weeks with ‘chronic stress’ - she had bruises all over her legs and couldn’t get out of bed. By the time they tested her, her neutrophils were at 320. Thank you for the clear signs list. Please share this with anyone on long-term NSAIDs or antibiotics. We need more awareness, not more silence.
Josh McEvoy January 29, 2026
bro i took naproxen for 3 months for my back and i felt like a ghost… thought i was just depressed lmao. now i know why i kept getting fevers and bleeding gums. i got a cbc last week and my platelets were low but not bad. i stopped the naproxen cold turkey and im already feeling less zombie-like. fyi: dont ignore the ‘i just feel tired’ phase. its not burnout, its your marrow screaming.
Sawyer Vitela January 31, 2026
Carbamazepine risk is 15x higher? Source? The FDA’s own data shows 0.7 per 100,000. That’s not 15x - that’s 0.0007%. You’re conflating relative risk with absolute risk. Alarmism without context is dangerous.
Shanta Blank February 2, 2026
Let me just say - this isn’t ‘rare.’ This is the quiet genocide of the overmedicated middle class. You take a pill for your headache, your anxiety, your arthritis - and boom, your body forgets how to make blood. And who gets blamed? YOU. For not ‘listening to your body.’ Meanwhile, Big Pharma quietly files their 10th 510(k) exemption for another bone marrow killer. This is systemic. And we’re all just collateral.
Tiffany Wagner February 3, 2026
i took gold injections for rheumatoid arthritis for 2 years and never knew this was a risk. i had random bruising but thought it was just aging. i wish i’d known sooner. i’m so glad this post exists. thanks for sharing the symptoms. i’ll get my blood checked next week.
Michael Camilleri February 3, 2026
You people act like medicine is poison but the real poison is ignorance. If you’re scared of every pill your doctor gives you then why even go to a doctor? The fact you think a CBC every month is normal tells me you’ve never lived in a country with real healthcare. This isn’t a conspiracy - it’s medicine. You take risks. You get tested. You live. Or you don’t. Stop screaming at the sky and start taking responsibility.
lorraine england February 4, 2026
Hi everyone - I’m a nurse in Chicago and I see this way more than you’d think. I’ve had patients come in with platelets under 10K and say they thought it was ‘just a cold.’ Please, if you’re on carbamazepine or sulfonamides - get that baseline CBC. It takes 5 minutes. And if your doctor says ‘it’s unlikely’ - ask them to write it down. You deserve to be heard. I’ve seen people live because they pushed. You can too ❤️
Darren Links February 4, 2026
Interesting how this post ignores that the U.S. has the highest per capita drug consumption in the world. We’re medicating everything - headaches, sadness, boredom - and then act shocked when our bodies break. Meanwhile, Europe has stricter toxicity testing. Guess which continent has lower rates of drug-induced aplastic anemia? Coincidence? I think not. We’ve turned our bodies into chemical test tubes and then blame the patient for the explosion.
Kevin Waters February 4, 2026
Just wanted to add - if you’re on any of these meds and you’re feeling off, don’t panic. But DO act. I had a patient who stopped ibuprofen at week 3, got tested, and caught it before it got bad. She’s now fully recovered after 6 weeks. It’s not always doom and gloom. Early = better. Simple as that. Keep a meds journal. Track symptoms. Trust your gut. You’re your own best advocate.
Kat Peterson February 6, 2026
OMG I literally just stopped my naproxen yesterday because I felt like I was dying 😭 I thought it was menopause. Turns out my ferritin was low and my platelets were borderline. I’m getting a full CBC tomorrow. This post literally saved me. I’m crying rn. Thank you. From a scared woman in LA who thought she was just ‘getting old.’
Helen Leite February 8, 2026
This is all a lie. The government and pharma are hiding the truth. They’re poisoning our water with fluoride and our meds with bone marrow killers so they can sell you transplants and chemo. I know someone who got this after taking Advil - he vanished. No autopsy. No records. They just say ‘aplastic anemia’ to cover it up. You think this is rare? It’s everywhere. They just don’t tell you. Google ‘CDC aplastic anemia coverup.’
Elizabeth Cannon February 10, 2026
My cousin had this after taking sulfamethoxazole for a UTI. She was 24. They thought it was flu. She ended up in ICU for 3 weeks. Got the transplant. Now she’s fine. But she can’t have kids because of the chemo. I told my mom to never let me take antibiotics without a blood test first. This isn’t hype. It’s real. And it hits young people too. Don’t wait. Get tested. Even if you feel ‘fine.’