When someone is trying to stop drinking, the hardest part isn’t always willpower - it’s the brain’s constant pull back toward alcohol. That’s where medications come in. For people with Alcohol Use Disorder (AUD), drugs like naltrexone, acamprosate, and disulfiram aren’t magic pills, but they do change the odds. Studies show they can cut relapse risk by 18% to 30%, depending on the person and the drug. Yet, only about 1 in 10 people with AUD in the U.S. even get prescribed one. Why? Because many don’t know how they work - or when they might make things worse.
How These Medications Actually Work
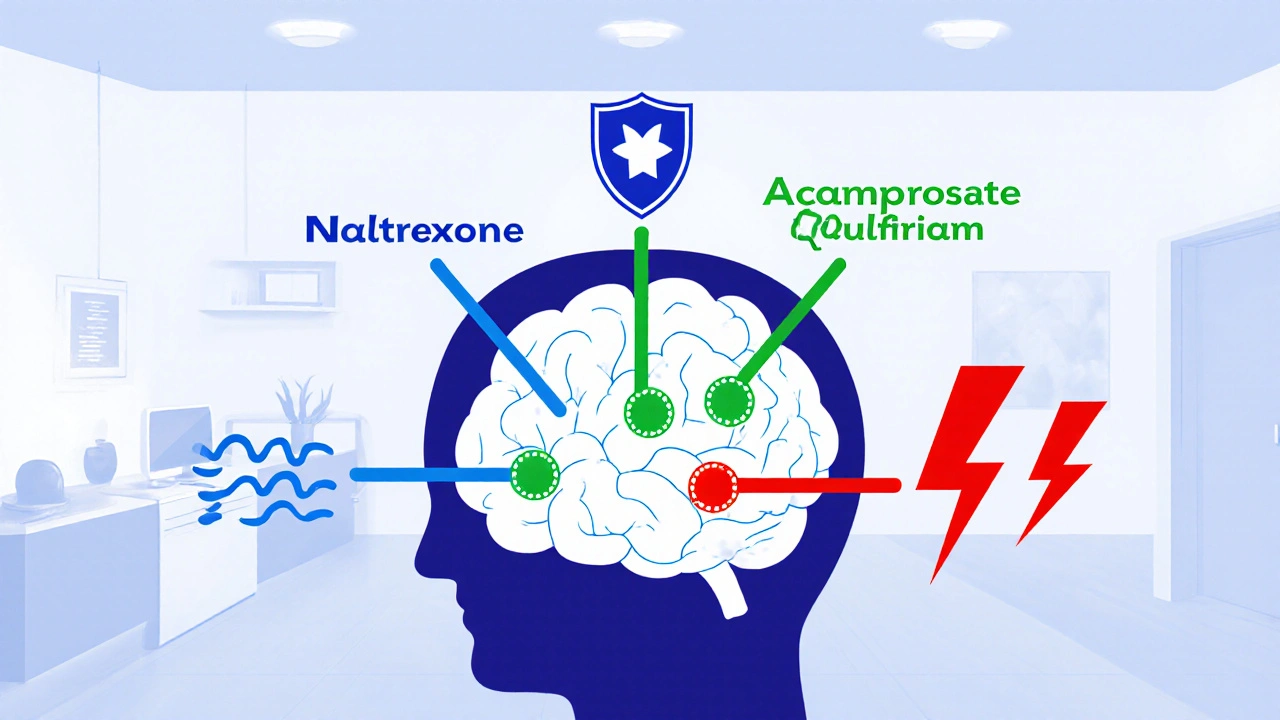
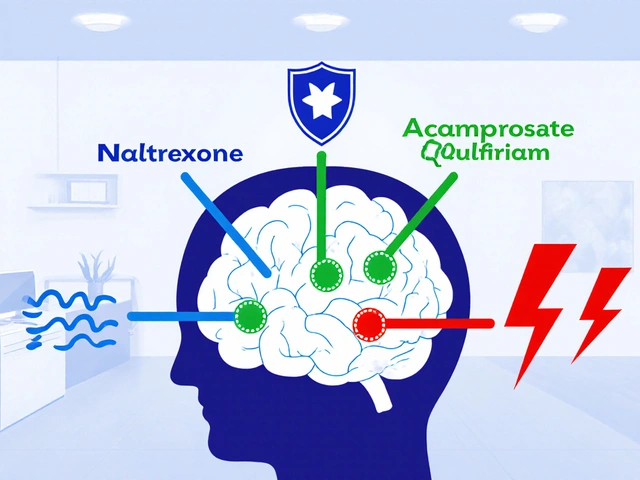
Each of the three FDA-approved medications for AUD targets a different part of the addiction cycle. They don’t cure alcohol dependence, but they help manage it - like insulin for diabetes.Naltrexone blocks the brain’s opioid receptors. When you drink, alcohol normally triggers a dopamine surge that makes you feel good. Naltrexone dulls that reward. You still drink, but it doesn’t feel as satisfying. That reduces heavy drinking episodes. A 2021 meta-analysis of nearly 3,000 people found oral naltrexone (50 mg daily) cut relapse risk by 18% compared to placebo. The monthly shot, Vivitrol, works the same way but doesn’t require daily pills.
Acamprosate works after you’ve stopped drinking. Heavy alcohol use scrambles brain chemicals like GABA and glutamate. When you quit, your brain stays out of balance, causing anxiety, restlessness, and insomnia - big triggers for relapse. Acamprosate helps stabilize those systems. It’s most effective for people who’ve already detoxed and are aiming for total abstinence. In clinical trials, it improved abstinence rates by about 15% over six months.
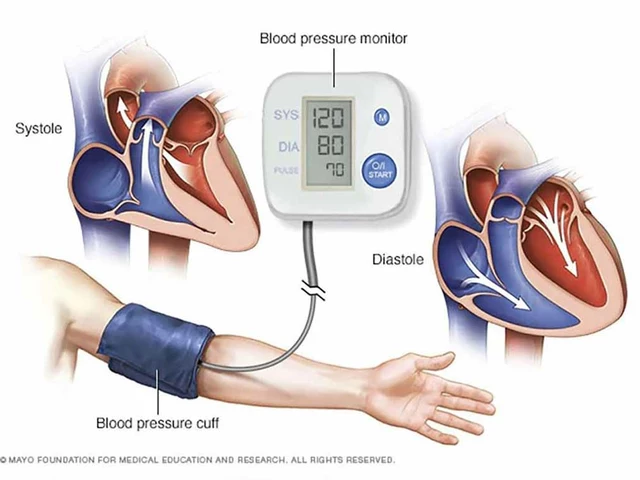
Disulfiram is the oldest and most dramatic. It makes your body react badly to alcohol. If you drink while taking it, you get intense flushing, nausea, vomiting, and a dangerous drop in blood pressure. It’s a deterrent - a physical warning sign that says, “Don’t even think about it.” But it only works if you take it consistently. And if you forget? The risk isn’t just a bad hangover - it’s a medical emergency.
Which Medication Is Right for You?
There’s no one-size-fits-all. The best choice depends on your goals, your body, and your history.If you’re trying to cut back on heavy drinking - maybe you’re not ready to quit completely - naltrexone is often the first pick. It doesn’t force abstinence. It just makes drinking less rewarding. People who’ve tried to quit before and kept falling back into binge patterns tend to respond well.
If you’ve already stopped drinking and want to stay stopped, acamprosate is the go-to. It helps with the emotional chaos that follows detox: the jitteriness, the irritability, the urge to drink just to feel normal. But here’s the catch: you can’t start it until you’ve been alcohol-free for at least 3 to 5 days. If you’re still drinking, it won’t help - and might even make you sick.
Disulfiram is for a very specific type of person: highly motivated, with strong social support, and willing to live with the consequences of a slip-up. It’s not for someone who drinks occasionally or is unsure about quitting. One study showed 28% of people quit disulfiram because of side effects like metallic taste, drowsiness, or fear of accidentally drinking something with alcohol - like mouthwash or cough syrup.
There’s also gabapentin, not FDA-approved for AUD but widely used off-label. It’s especially helpful for people who’ve had severe withdrawal symptoms - seizures, hallucinations, delirium tremens. A 2020 trial found 45% of high-risk patients stayed abstinent on gabapentin, compared to 28% on placebo. It’s also safer for people with liver disease, since it’s cleared by the kidneys, not the liver.
Why So Many People Stop Taking These Drugs
The data is clear: these medications work. But real life is messier.In clinical trials, about 60% of people stick with naltrexone or acamprosate for 16 weeks. In the real world? Only 35% are still taking them after three months. Why?
- Side effects: Nausea is common with naltrexone. Diarrhea and dizziness happen with acamprosate. Disulfiram causes fatigue and a bad taste in the mouth.
- Cost: Even though most are available as generics, monthly costs can hit $200-$400. Insurance doesn’t always cover them, and copays add up fast.
- Timing: You can’t start acamprosate until you’ve stopped drinking. If you’re still using, you’re stuck waiting - and that waiting period is when most people slip back.
- Expectations: Many think medication will make the craving disappear. It doesn’t. It just makes drinking less appealing. If you’re expecting a miracle, you’ll be disappointed.
One patient told a recovery forum: “I took naltrexone for two months. I didn’t get drunk, but I still drank every night. It didn’t make me stop - just made me feel weird.” That’s not failure. That’s how it works. The goal isn’t to feel nothing. It’s to reduce the damage.

What Happens When You Mix Medication With Alcohol
This is where things get dangerous.With disulfiram, drinking even a small amount of alcohol - a sip of wine, a beer, or a dessert with alcohol - can trigger a life-threatening reaction. Blood pressure can crash. Heart rhythm can go haywire. Emergency rooms see this often.
With naltrexone, drinking isn’t physically dangerous, but it defeats the purpose. You’ll still get the physical effects of alcohol - impaired coordination, poor judgment - but you won’t feel the usual reward. That can lead to risky behavior: “I’m on naltrexone, so I’ll have more.” That increases the chance of injury or overdose.
With acamprosate, alcohol doesn’t cause a bad reaction. But if you drink while taking it, the medication doesn’t work. It’s like taking insulin and then eating a whole cake - the drug can’t fix what you’re actively breaking.
And then there’s liver damage. Naltrexone is processed by the liver. If you have cirrhosis or hepatitis, it can build up and cause toxicity. Doctors check liver enzymes before and during treatment. Acamprosate is cleared by the kidneys - so if you have kidney disease, your dose must be lowered. Gabapentin is safer here, which is why it’s becoming a top choice for people with alcohol-related liver disease.
Why So Few Doctors Prescribe These Drugs
You might think, “If they work, why isn’t everyone on them?” The answer is simple: most doctors don’t know how to use them.A 2023 survey found only 28% of primary care doctors in the U.S. feel confident prescribing AUD medications. Many still think addiction treatment belongs only in rehab centers or specialty clinics. But AUD is a medical condition - like high blood pressure or diabetes. It should be treated in the same place you go for your annual checkup.
Doctors also worry about liability. If someone on disulfiram drinks and ends up in the ER, who’s responsible? If a patient on naltrexone keeps drinking and loses their job, did the doctor enable it?
But the bigger problem is stigma. Addiction is still seen as a moral failure, not a brain disease. That’s changing - slowly. More medical schools now teach addiction medicine. More insurance plans are covering AUD meds. But progress is uneven.
What’s Next: New Treatments and Personalized Care
The field is moving fast.Researchers are using brain scans to predict who will respond to which drug. One study found that people with higher white matter integrity in the frontal brain region were 68% more likely to respond to acamprosate. That means one day, we might test your brain before prescribing.
New drugs are coming. A combination of buprenorphine and samidorphan reduced heavy drinking days by 32% in a 2023 trial. Ketamine infusions showed a 41% drop in relapse. Even probiotics and anti-inflammatory agents are being tested, because gut health is linked to cravings.
Longer-acting forms are also in development. A 6-month naltrexone implant is in phase 2 trials. If it works, adherence could jump from 42% (with monthly shots) to 78%. That’s huge.
And digital tools are helping. Apps that track cravings, send reminders, and connect you to peer support have been shown to cut relapse risk by a third when used with medication.
What You Can Do Right Now
If you or someone you know is struggling with alcohol:- Don’t wait for “rock bottom.” Medications work best when started early.
- Ask your doctor about naltrexone or acamprosate. They’re safer and more effective than you think.
- If you’ve had withdrawal symptoms before, ask about gabapentin.
- If you’re considering disulfiram, make sure you have strong support - and understand the risks.
- Don’t stop taking the medication just because you feel fine. Most people relapse within months of quitting.
- Combine medication with counseling. No pill works alone.
Alcohol Use Disorder isn’t a character flaw. It’s a medical condition with proven treatments. The fact that so few people get them isn’t because the treatments don’t work. It’s because we still don’t treat addiction like the disease it is.
Can I drink alcohol while taking naltrexone?
Yes, you can - but it defeats the purpose. Naltrexone blocks the pleasurable effects of alcohol, so drinking becomes less rewarding. But it doesn’t protect you from alcohol’s physical harm - impaired judgment, liver damage, or overdose risk. Some people drink more to overcome the block, which increases danger. The goal is to reduce drinking, not to drink heavily while medicated.
How long should I take AUD medications?
Most guidelines recommend 6 to 12 months. But for many people, AUD is a chronic condition - like hypertension or asthma. Stopping too soon increases relapse risk. Some patients stay on naltrexone or acamprosate for years. The key is to work with your doctor to decide when it’s safe to taper, not to quit on your own.
Why isn’t disulfiram used more often?
Because it’s hard to use safely. The reaction to alcohol can be severe - even life-threatening. Patients often stop taking it because of side effects like drowsiness or a bad taste. Compliance is low, and studies on its effectiveness have methodological flaws. It’s only recommended for highly motivated patients with strong support systems - not for most people.
Can I take these medications if I have liver disease?
It depends. Naltrexone is processed by the liver, so it’s risky if you have cirrhosis or active hepatitis. Acamprosate is cleared by the kidneys, so it’s safer for liver disease - but kidney function must be checked. Gabapentin is often preferred in these cases because it doesn’t stress the liver. Always get liver tests before starting any medication.
Are there any new medications for AUD on the horizon?
Yes. A 6-month naltrexone implant is in late-stage trials and could improve adherence dramatically. A combination drug called ALKS 5461 reduced heavy drinking by 32% in a 2023 trial. Ketamine infusions and gut-targeted therapies like probiotics are also showing promise. These aren’t available yet, but they’re coming fast - and they’re based on real science, not hype.
Do these medications help with cravings?
Naltrexone reduces cravings by blocking the brain’s reward system. Acamprosate helps by calming brain activity after withdrawal, which lowers the emotional urge to drink. Gabapentin reduces anxiety-related cravings, especially in people with a history of severe withdrawal. No medication eliminates cravings completely - but they can make them manageable.
If you’ve tried to quit drinking before and failed, don’t give up. The problem isn’t you - it’s that you haven’t found the right tool yet. Medications for AUD aren’t perfect, but they’re the most effective option we have. And they work best when you’re not alone.





Savakrit Singh November 26, 2025
Interesting breakdown, but let’s be real - most of these meds are just fancy placebos with side effects. 🤷♂️ Naltrexone? Makes you feel like a zombie. Acamprosate? Costs more than my rent. And disulfiram? That’s not treatment, that’s punishment. We need better options, not more chemical handcuffs. 💊😭
Cecily Bogsprocket November 28, 2025
I’ve been on naltrexone for 14 months now. It didn’t make me ‘cured,’ but it made me stop needing to drink to feel okay. The craving didn’t vanish - it just lost its scream. I still have bad days. But now I have space to choose. That’s everything.
It’s not about willpower. It’s about rewiring. And this isn’t a moral failure. It’s neurobiology. We treat diabetes with insulin - why are we still whispering about AUD?
Also, gabapentin changed my life. No more night terrors. No more trembling hands at 3 a.m. If you’ve had withdrawal, ask your doctor. Don’t wait until you’re broken.
And yes - it’s okay to stay on it for years. No shame. No rush. Healing isn’t a sprint.
Thank you for writing this. So many people need to hear it.
Jebari Lewis November 28, 2025
Wait - you’re telling me doctors don’t know how to prescribe these? That’s absurd. We have peer-reviewed meta-analyses, FDA approvals, and clinical guidelines - yet primary care physicians are still treating addiction like it’s a 1950s moral dilemma?
This isn’t just negligence. It’s systemic failure. We train doctors to manage hypertension, but when someone’s brain chemistry is hijacked by alcohol? They get shrugged off.
And don’t get me started on insurance. Why is naltrexone a $300 copay when metformin is $4? This is healthcare apartheid.
Also - gabapentin for liver patients? Brilliant. Why isn’t this first-line? The data’s there. The safety profile’s better. Why are we still clinging to disulfiram like it’s a medieval exorcism?
We need mandatory addiction training in med school. Not optional. Not ‘if you’re interested.’ Required. Like CPR.
Emma louise November 30, 2025
Oh wow. So now we’re medicalizing weakness? Next you’ll tell me people who eat too much cake have a ‘sugar use disorder’ and need a prescription.
Alcoholism isn’t a disease - it’s a choice. A lazy, selfish, entitled choice. If you can’t stop drinking, maybe you’re just not trying hard enough. Why should I pay for your ‘treatment’ with my taxes?
And ‘gabapentin’? That’s just a painkiller for people who can’t handle life. Pathetic.
Alex Hess December 1, 2025
This is the most overwrought, jargon-filled, pseudo-scientific fluff I’ve read in months. ‘White matter integrity’? ‘Gut-brain axis’? You sound like a grad student who just discovered PubMed.
Most people who drink too much just need discipline. Not a 6-month implant. Not a brain scan. Not a goddamn probiotic.
And ‘don’t wait for rock bottom’? Who says we should even help people until they’ve hit it? Maybe if they lost their job, their family, their house - they’d finally grow up.
This isn’t medicine. It’s therapy for the entitled.
Leo Adi December 1, 2025
From India - we don’t have access to any of these. Naltrexone? Unavailable. Acamprosate? Only in big city hospitals. And disulfiram? Too dangerous for our healthcare system.
So we use Ayurveda. Ashwagandha. Brahmi. Some swear by it. Others say it’s placebo. But it’s all we have.
Still - your point about stigma? 100% true here too. Families hide it. No one talks. ‘He’s just a drunk’ - that’s the whole diagnosis.
Thank you for writing this. Someone needed to say it.
Melania Rubio Moreno December 1, 2025
so like… if you take naltrexone and still drink… does it just make you feel kinda… meh? like, you’re drunk but also bored? 🤔
steve stofelano, jr. December 3, 2025
As a physician who has treated AUD for over two decades, I can attest to the profound efficacy of these pharmacotherapies when properly administered. The notion that addiction is a moral failing is not only scientifically inaccurate but also ethically indefensible.
Naltrexone, acamprosate, and gabapentin are not merely adjuncts - they are foundational interventions that restore neurochemical equilibrium in a brain pathologically altered by chronic alcohol exposure.
The barriers to access are not technical but ideological. We have the tools. We lack the collective will to treat this condition with the same urgency as myocardial infarction or metastatic cancer.
Furthermore, the emerging data on long-acting formulations and neuroimaging-guided prescribing represent a paradigm shift - one that will, in time, render the current fragmented model obsolete.
It is not enough to hope for change. We must legislate it. Reimburse it. Teach it. And above all - normalize it.
Thank you for this lucid, evidence-based exposition. It is precisely the kind of discourse our field requires.
Sam HardcastleJIV December 4, 2025
One must ask: if these medications reduce relapse by 18–30%, then what is the baseline? Is the placebo effect not also a form of neurobiological intervention? And if the goal is abstinence, why not simply promote total sobriety through behavioral conditioning, as has been done for centuries?
The medicalization of human behavior, while seemingly compassionate, often obscures deeper existential and sociocultural roots. Is the desire to drink truly a disorder - or a symptom of alienation in a hyper-individualistic society?
Moreover, the financial burden of these treatments is rarely discussed in the context of global inequity. Who bears the cost? Who is excluded? And who profits?
One must tread carefully before turning human suffering into a pharmaceutical commodity.
Mira Adam December 4, 2025
Oh please. You act like these drugs are magic. But what about the people who take them and still drink? What about the ones who feel worse on them? What about the ones who can’t afford them, or can’t get them because their doctor doesn’t ‘believe’ in addiction medicine?
You talk about brain scans and implants like they’re the future - but most people can’t even get a refill because their pharmacy ran out of naltrexone.
This isn’t science. It’s wishful thinking dressed up in jargon. And you know what? People aren’t stupid. They can smell the hype.
Maybe the real problem isn’t the meds - it’s that we keep pretending there’s a quick fix for something that requires real, messy, lifelong work.
Miriam Lohrum December 4, 2025
I’ve been sober for 7 years. Took naltrexone for 11 months. Didn’t need it after that - but it gave me the breathing room to build a life without alcohol.
It’s not about the pill. It’s about what the pill gives you: time. Space. A pause between the urge and the action.
That pause? That’s where recovery happens.
Thank you for writing this. It’s rare to see the nuance.
Cecily Bogsprocket December 5, 2025
Thank you for saying that - about the pause. That’s exactly it.
I used to think if I just had more willpower, I’d stop. But willpower isn’t a muscle you strengthen - it’s a resource that gets drained by stress, trauma, sleep loss, loneliness.
Naltrexone didn’t make me want to quit. It just made it possible to say ‘no’ when I was too tired to fight.
That’s not magic. That’s mercy.