Heart failure isn’t just about a weak heart. It’s about a body struggling to keep up, and the medications that help it do so come with serious monitoring requirements. If you’re on one or more of these drugs, skipping check-ups or ignoring symptoms isn’t just risky-it can be life-threatening. The four cornerstone medications for heart failure with reduced ejection fraction (HFrEF)-ARNIs, beta-blockers, MRAs, and SGLT2 inhibitors-are powerful, but they don’t work the same for everyone. And when you’re older, have kidney issues, are a woman, or belong to certain ethnic groups, the risks change. Monitoring isn’t a box to tick. It’s the difference between getting better and ending up back in the hospital.
Why Monitoring Isn’t Optional
Heart failure affects 6.2 million Americans, and nearly 1 million are hospitalized each year because their treatment didn’t work-or made things worse. The problem isn’t always the drugs. It’s that most patients never get to the right dose. Only 30-40% of eligible patients receive all four recommended medications at target levels. Why? Because doctors and patients are scared of side effects, especially when labs go off track. But here’s the truth: not taking these meds at the right dose is far more dangerous than managing the side effects.
For example, mineralocorticoid receptor antagonists (MRAs) like spironolactone and eplerenone cut death risk by 30% in HFrEF patients. But 68% of eligible patients never start them because of fear of high potassium. That fear isn’t baseless-but it’s often overblown. With proper monitoring, MRAs are safe. The key is knowing when to check, how often, and what to do if numbers rise.
Beta-Blockers: Slowing the Heart to Save It
Beta-blockers like carvedilol, bisoprolol, and metoprolol succinate don’t just lower blood pressure. They slow your heart rate so your heart doesn’t wear out. The goal? A resting heart rate between 50 and 60 beats per minute. That’s slower than most people think is normal-and it’s exactly what saves lives.
But you can’t start at the full dose. You begin low and go slow. Check your pulse weekly. If it drops below 50 and you feel dizzy or tired, call your doctor. Don’t stop the pill. Dose adjustments are normal. The 2024 ACC guidelines say if your heart rate stays above 70 even on the highest tolerated beta-blocker dose, ivabradine might be added. But here’s the catch: ivabradine isn’t for everyone. If you have angina, it raises your risk of heart problems by 28%. And if you’re over 75 or have a slow heart rhythm, the dose must be cut in half-to 2.5 mg twice daily.
Real-world data shows only 22% of patients get beta-blockers at target doses. Why? Too many stop because they feel tired. But fatigue often fades after a few weeks. The real test is whether your energy improves over time. If not, talk to your doctor. Don’t quit.
MRAs: The Potassium Tightrope
MRAs are the most monitored drugs in heart failure. Why? Because they can raise potassium levels-and high potassium can stop your heart.
Before starting an MRA, your doctor should check your potassium and kidney function. Then, check again in 3 to 7 days. After that, every 3 to 6 months. That’s non-negotiable. But here’s what many don’t tell you: non-Caucasian patients are 75% more likely to develop dangerous hyperkalemia than White patients. Women also have higher drug exposure. That means your monitoring schedule might need to be tighter than your neighbor’s.
If your potassium rises above 5.5 mmol/L, your doctor may pause the MRA and adjust your diuretic. But don’t panic. A small rise doesn’t mean you can’t take it again. Many patients get back on MRAs safely after a short break. The goal isn’t to avoid high potassium forever-it’s to manage it so you keep the life-saving benefits.
And yes, this is why so many patients never start MRAs. But studies show that with structured monitoring programs-like pharmacist-led check-ins or EHR alerts-discontinuation drops by 35%. You don’t have to be scared. You just need a plan.

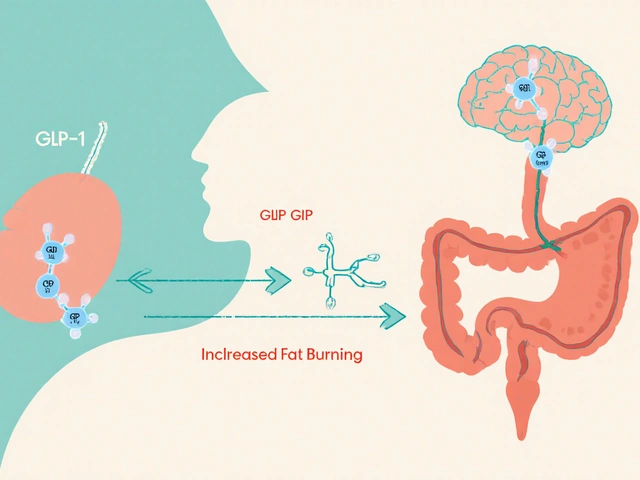
SGLT2 Inhibitors: The New Kid on the Block
Once used only for diabetes, SGLT2 inhibitors like dapagliflozin and empagliflozin are now first-line for all types of heart failure-even if you don’t have diabetes. They reduce hospitalizations by 30% and lower death risk. And here’s the best part: they need far less monitoring than MRAs or ACE inhibitors.
But they’re not risk-free. The most common issue? Genital yeast infections. In trials, 11.9% of people on SGLT2 inhibitors got them-nearly triple the placebo rate. If you’re a woman or have trouble with hygiene, this matters. Keep the area dry, wear cotton underwear, and tell your doctor if you notice itching or burning. It’s treatable, not a reason to stop.
Bigger concern: diabetic ketoacidosis (DKA). Even if your blood sugar is normal. Yes, that’s real. It’s rare, but it happens more in people who are dehydrated, sick, or on very low-carb diets. If you feel nauseous, vomit, or have fruity-smelling breath, get checked immediately. No waiting.
And if you’re over 75? Watch your fluid intake. SGLT2 inhibitors make you pee more. If you’re on strong diuretics or have low blood pressure, you could get too dry. Your doctor should check your weight weekly for the first month. A 2-kg drop? That’s a red flag.
Despite being recommended for 50% of heart failure patients now, only 58% of eligible people are monitored properly. That’s a gap. Don’t let yours be one of them.
ARNIs: Blood Pressure and the First Two Weeks
ARNIs like sacubitril-valsartan replaced ACE inhibitors for many patients because they work better. But they come with a warning: they can drop your blood pressure hard-especially in the first two weeks.
In the PARADIGM-HF trial, 14% of people on sacubitril-valsartan had symptoms of low blood pressure-dizziness, fainting, fatigue-compared to 9.2% on enalapril. That’s not rare. It’s expected. So what do you do? Don’t stop the pill. But do check your blood pressure at home, twice a day, for the first 14 days. If your systolic number drops below 90 and you feel lightheaded, call your doctor. You might need a lower dose or a pause.
Also, women have about 30% higher exposure to sacubitril-valsartan than men. That means you might need a slower titration. And if you’ve had angioedema with an ACE inhibitor before? Don’t take ARNIs. That’s a hard no.
Special Populations: One Size Doesn’t Fit All
Heart failure isn’t the same for everyone. Your age, gender, race, and kidney function change how these drugs affect you.
- Over 75? Start ivabradine at 2.5 mg twice daily. Don’t go straight to 5 mg. Your body processes drugs slower.
- Woman? You may need lower ARNI doses. Your weight and metabolism differ from men’s.
- Non-Caucasian? Higher risk of high potassium on MRAs. Monitor more often.
- Chronic kidney disease? SGLT2 inhibitors still help-but your dose may need adjusting. Never start if your eGFR is below 20 without specialist input.
- On multiple meds? 37% of patients on four heart failure drugs have side effects. Watch for dizziness, fatigue, or swelling. It might be the combo, not just one pill.
There’s no universal plan. Your monitoring schedule should be as unique as your fingerprint.
What’s New in 2026?
Monitoring is getting smarter. AI tools now predict high potassium with 83% accuracy by scanning your lab history, diet, and other meds. Some pharmacies offer free home potassium test kits for MRA patients. And new patches-still in trials-can track potassium continuously, replacing monthly blood draws.
Remote monitoring is growing. Implantable sensors that track lung pressure (like in the CHAMPION trial) cut hospitalizations by 30%. But only 1.2% of eligible patients have them. Why? Cost, access, and lack of training. Still, if you’ve been hospitalized for heart failure in the last year, ask your doctor if you’re a candidate.
And the future? By 2030, your heart failure meds will be chosen based on your genes, your lifestyle, and your kidney health-not just your ejection fraction. Personalized monitoring won’t be optional. It’ll be standard.
What You Can Do Today
You don’t need a fancy device or a tech-savvy doctor to stay safe. Here’s your simple checklist:
- Know your meds. Write down what you take, why, and what dose.
- Check your pulse weekly. If it’s under 50 and you feel weak, call your doctor.
- Track your weight daily. A 2 kg gain in 3 days? That’s fluid. Call your doctor.
- Know your potassium numbers. If you’re on an MRA, ask when your next test is. Don’t wait for them to call you.
- Report yeast infections, nausea, or dizziness. Don’t assume it’s normal.
- Ask if you’re on all four GDMT drugs at target doses. If not, ask why.
Heart failure meds are not set-and-forget. They need attention. But with the right monitoring, they can give you years-not just months-of better life.
How often should potassium be checked when taking an MRA for heart failure?
Before starting an MRA like spironolactone or eplerenone, your doctor should check your potassium and kidney function. Then, check again within 3 to 7 days after starting or increasing the dose. After that, monitor every 3 to 6 months if your levels are stable. If you have kidney disease, are older, or are non-Caucasian, your doctor may check more often-sometimes monthly at first.
Can I take SGLT2 inhibitors if I don’t have diabetes?
Yes. SGLT2 inhibitors like dapagliflozin and empagliflozin are now recommended for all heart failure patients with reduced or preserved ejection fraction-even if you don’t have diabetes. They reduce hospitalizations and improve survival regardless of blood sugar levels. The FDA approved dapagliflozin for heart failure without diabetes in 2021, and guidelines expanded in 2022 to include HFpEF.
Why do I need to check my blood pressure after starting an ARNI?
ARNIs like sacubitril-valsartan can cause a sudden drop in blood pressure, especially in the first two weeks. About 14% of patients experience symptoms like dizziness or fainting. Checking your blood pressure at home during this time helps catch low pressure early. If your systolic number falls below 90 and you feel unwell, call your doctor. You may need a lower dose, but don’t stop the medication without talking to them.
Is it safe to take ivabradine with a beta-blocker?
Yes, but only if your heart rate stays above 70 beats per minute despite the highest tolerated beta-blocker dose. Ivabradine slows the heart further and is often added in these cases. But it’s not for everyone. Avoid it if you have angina-it increases ischemic risk by 28%. Also, if you’re over 75 or have a slow heart rhythm, start at half the dose (2.5 mg twice daily). Never take it with strong CYP3A4 inhibitors like clarithromycin or grapefruit juice.
What should I do if I miss a dose of my heart failure medication?
If you miss a dose, take it as soon as you remember-if it’s within a few hours. If it’s almost time for your next dose, skip the missed one. Don’t double up. For MRAs or ARNIs, missing doses can lead to fluid buildup or rising blood pressure. For SGLT2 inhibitors, occasional misses are less risky, but consistency improves outcomes. Use a pill organizer or phone reminder. If you miss more than two doses in a week, talk to your doctor. They may adjust your plan.
Can I stop my heart failure meds if I feel better?
No. Feeling better is a sign the meds are working-not that you no longer need them. Stopping beta-blockers, MRAs, or ARNIs suddenly can cause your heart failure to worsen rapidly, even leading to sudden death. SGLT2 inhibitors also need to be continued long-term. If you’re having side effects, talk to your doctor. They can adjust the dose or switch you to another medication. Never stop on your own.
Next Steps: What to Ask Your Doctor
Before your next appointment, write down these questions:
- Am I on all four GDMT medications at target doses?
- When is my next potassium test? Do I need one sooner?
- Should I check my blood pressure at home? How often?
- Are there any signs I should watch for that mean I need to call you right away?
- Do I need a home weight scale? How much weight gain should worry me?
Heart failure treatment has come a long way. But progress only matters if you’re monitored properly. You’re not just taking pills. You’re managing a system. And that system needs your attention every day.






Layla Anna January 2, 2026
i just started on spironolactone and honestly i was terrified of the potassium thing but my pharmacist gave me a free home test kit and now i check it every week like a habit 😅 i feel way more in control than before
also the yeast infections from the SGLT2? yeah that happened to me but cotton underwear and no tight jeans fixed it. no biggie.
Heather Josey January 3, 2026
This is one of the most comprehensive and clinically accurate summaries I’ve read on heart failure pharmacotherapy. The emphasis on individualized monitoring-particularly for non-Caucasian patients and women-is not just important, it’s essential. Too many guidelines still treat heart failure as a one-size-fits-all condition. The data on MRA discontinuation due to fear of hyperkalemia is alarming, and the 35% reduction in discontinuation with structured programs should be standard protocol nationwide. Thank you for highlighting the role of pharmacists and EHR alerts-these are scalable solutions that save lives.
Donna Peplinskie January 4, 2026
I just want to say… thank you… for writing this… with such care… and clarity…
My mom has HFrEF… and she was on three meds… but didn’t know about the fourth… SGLT2… until I found this article… and now… she’s on it… and her energy is better… and she’s not as swollen…
And yes… she checks her weight… every morning… like you said… and she writes it down… in her little notebook… with a red pen… for the days it goes up…
She’s 81… and she’s still walking to the mailbox… and that… is everything…
Olukayode Oguntulu January 5, 2026
Ah, the neoliberal pharmacopeia-reifying biomedical hegemony under the guise of patient empowerment. You speak of ‘monitoring’ as if it’s a neutral act, but let us interrogate the epistemic violence embedded in the algorithmic surveillance of potassium levels. Who benefits? Pharma. Who bears the burden? The elderly, the marginalized, the non-Caucasian bodies rendered hyper-visible through EHR alerts and home test kits. The ‘personalized’ monitoring you extol is merely the commodification of vulnerability. The real solution? Defund the cardiac industrial complex and invest in community-based care. But no-better to sell more SGLT2 inhibitors and call it progress.
jaspreet sandhu January 6, 2026
You people act like these drugs are magic pills but the truth is most of them do more harm than good. My uncle took all four and ended up in ICU with low blood pressure and high potassium. He was 76. They told him to keep going but he got worse. Now he’s on oxygen. So don’t tell me about target doses. Target doses are for people who don’t know what real life looks like. I’ve seen it. It’s not about following guidelines. It’s about survival. And sometimes survival means not taking the pills at all. The doctors don’t tell you that part. They just want you to sign the consent form.
Alex Warden January 7, 2026
This is why America’s healthcare is broken. You’re telling people to check potassium every week like it’s a chore? In my day, you took your meds and didn’t complain. Now we got apps, home tests, patches, AI, and 17 different blood draws a month. It’s overkill. My grandpa took his pills once a day and lived to 92. He didn’t need a PhD to manage his heart. Just a strong will and a good doctor. Stop overmedicalizing everything. Less monitoring, more discipline.
LIZETH DE PACHECO January 8, 2026
I’m a nurse and I see this every day. Patients stop their meds because they’re scared or tired or overwhelmed. But the thing is-they’re not alone. If you’re on any of these drugs, reach out. Text your local heart failure clinic. Ask for a care coordinator. Most hospitals have free support groups. You don’t have to do this alone. And if you’re feeling guilty about missing a dose? Don’t. Just call. One phone call can change everything. You’re not failing. You’re human. And that’s okay.
Lee M January 10, 2026
The real issue isn’t monitoring. It’s that we’ve turned heart failure into a numbers game. Pulse, potassium, weight, eGFR-everything reduced to digits. But the heart isn’t a lab report. It’s a living thing. And the people who live with it? They’re not patients. They’re people. You can’t optimize a soul with an algorithm. The future isn’t in patches or AI. It’s in presence. In someone sitting with you, not just checking your labs. That’s what’s missing.