Nov, 13 2025
|
10 Comments
When your kidneys suddenly stop working like they should, it’s not a slow fade-it’s a crash. Acute Kidney Injury (AKI) doesn’t wait for a warning sign. One day you feel fine; the next, you’re swollen, tired, and confused. And in many cases, you won’t even realize it’s happening until a routine blood test shows your creatinine has spiked. This isn’t just a lab anomaly. It’s a medical emergency that can turn deadly in hours if ignored.
What Actually Happens When Your Kidneys Shut Down
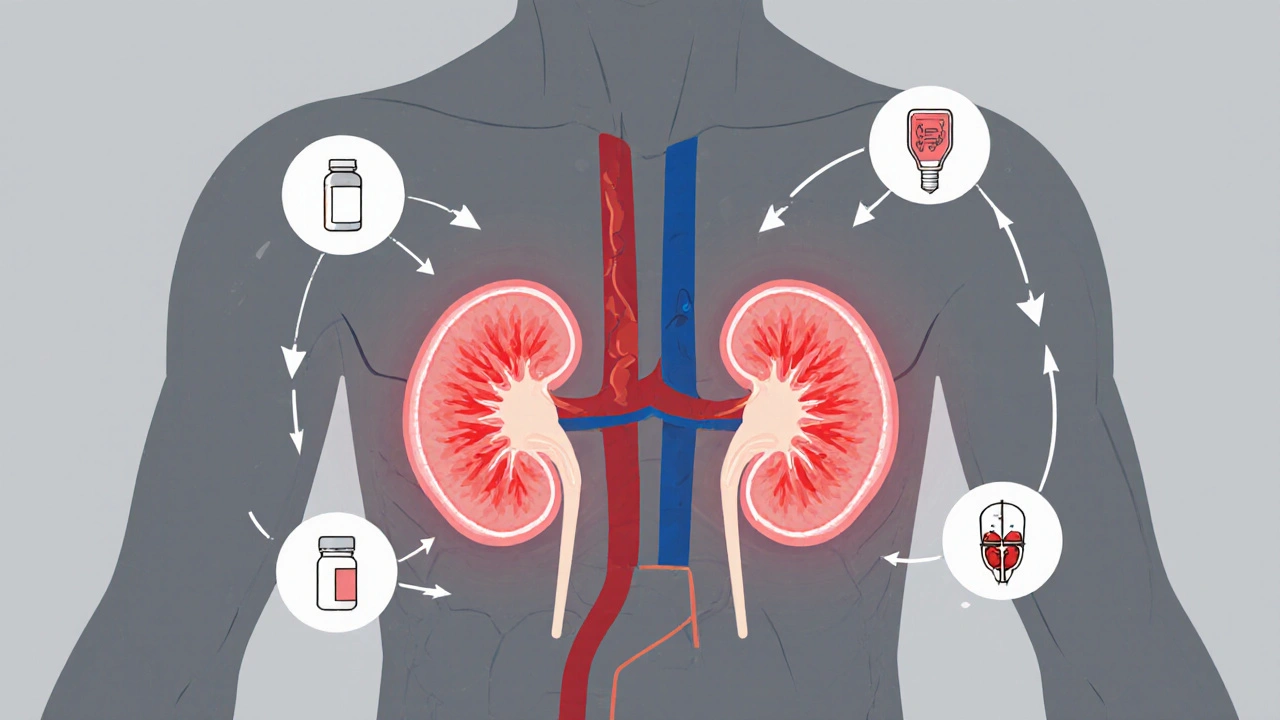
Your kidneys don’t just make urine. They filter 120-150 quarts of blood every day, removing waste, balancing salts, and keeping your blood pressure steady. When AKI hits, that system breaks down fast. Within hours or days, your kidneys lose the ability to clear toxins, regulate fluids, and control electrolytes like potassium and sodium.
The key is understanding this isn’t one disease-it’s a group of problems with different causes. About 60-70% of cases are prerenal: your kidneys aren’t getting enough blood. That can happen from severe dehydration after vomiting or diarrhea, major blood loss after an injury, or heart failure dropping your blood pressure below 90 mmHg for more than an hour. Your kidneys aren’t broken-they’re starving.
Then there’s intrarenal AKI, which makes up 25-35% of cases. Here, the kidney tissue itself is damaged. The most common cause? Acute tubular necrosis (ATN), where the tiny filtering tubes inside the kidney die off. This often comes from antibiotics like gentamicin, contrast dye used in CT scans, or severe infections like sepsis. Glomerulonephritis, an inflammation of the kidney’s filtering units, is another culprit, especially in people with autoimmune diseases like lupus.
Postrenal AKI, the least common but easiest to fix, accounts for 5-10% of cases. Something is blocking urine flow-like an enlarged prostate in older men, kidney stones blocking both ureters, or a tumor pressing on the bladder. If you can remove the blockage, the kidneys often bounce back fast.
How You’ll Know Something’s Wrong (And When You Won’t)
The scary part? You might not feel anything.
About 22% of AKI cases show no symptoms at all. They’re caught only because a doctor ordered blood work during a hospital stay. But when symptoms do appear, they’re hard to ignore.
Most people notice they’re peeing less-under 400 mL a day (oliguria) or even under 100 mL (anuria). But some, especially with blockages, keep making normal amounts of urine. That’s why urine output alone isn’t enough.
Fluid builds up fast. You’ll see swelling in your legs, ankles, or feet. You might feel short of breath because fluid is filling your lungs. Fatigue hits hard-75% of patients report extreme tiredness. Nausea, confusion, chest pain, and flank pain (between your ribs and hips) are also common.
In older adults, confusion can be the only sign. It’s often mistaken for dementia or a stroke. But if you’ve had a recent infection, surgery, or started a new medication, AKI could be the real culprit.
How Doctors Diagnose It-Fast
There’s no single test for AKI. Diagnosis relies on three things: blood tests, urine output, and imaging.
The gold standard? Serum creatinine. A rise of 0.3 mg/dL in 48 hours-or a 50% jump from your baseline over 7 days-means AKI. Your baseline matters. If your normal creatinine is 0.8, a jump to 1.2 is serious. If your baseline is 1.5 (because you have chronic kidney disease), a rise to 2.2 is still AKI, but it’s not as dramatic.
Urine output is tracked hourly in hospitals. Less than 0.5 mL per kg of body weight per hour for 6 hours? That’s a stage 1 AKI. Less than 0.3 mL/kg/h for 24 hours? That’s stage 3-the most severe.
Blood tests also check BUN (blood urea nitrogen). A BUN over 20 mg/dL and a high BUN-to-creatinine ratio often point to prerenal causes. A low fractional excretion of sodium (FeNa) under 1% also suggests your kidneys are conserving fluid due to low blood flow.
Ultrasound is used in 85% of cases. It shows if your kidneys are enlarged (a sign of obstruction) or shrunken (a sign of long-term damage). If a stone is suspected, a CT urogram can spot it with 95% accuracy.
New tools are coming. Biomarkers like NGAL and TIMP-2/IGFBP7 can predict AKI 24-48 hours before creatinine rises. Hospitals in Toronto and Pittsburgh are already using them in ICUs to catch cases before they spiral.

Treatment: It’s All About the Cause
There’s no magic pill for AKI. Treatment is all about fixing what broke it.
For prerenal AKI, it’s simple: give fluids. A 500-1000 mL IV saline bolus often brings creatinine back down in 24 hours. If it’s heart failure causing low blood pressure, diuretics and heart meds are added. If it’s sepsis, antibiotics and vasopressors are started immediately.
For intrarenal AKI, the first step is stopping the poison. If a drug like vancomycin or contrast dye caused it, you stop it. If it’s glomerulonephritis, you need steroids or immunosuppressants. For hemolytic uremic syndrome, plasmapheresis-filtering and cleaning the blood-can save kidneys if done within 24 hours.
For postrenal AKI, it’s a race against time. A ureteral stent placed under ultrasound guidance can restore urine flow in minutes. For an enlarged prostate, a catheter relieves pressure fast. If a tumor is blocking the ureter, a stent or nephrostomy tube can buy time until surgery.
If things get bad-high potassium, fluid in the lungs, acid buildup-you need dialysis. About 5-10% of hospitalized AKI patients need it. Hemodialysis is common. In the ICU, continuous renal replacement therapy (CRRT) is used for unstable patients. It’s slower, gentler, and keeps blood pressure steady.
Recovery: It’s Not Guaranteed
Most people think if you survive AKI, you’re fine. That’s not true.
Prerenal AKI? If caught early, 70-80% recover full kidney function within 7-10 days. No long-term damage.
Intrarenal AKI? It’s messier. If it’s mild ATN, 40-60% recover over 2-6 weeks. But if you were oliguric for more than two weeks, only 20-30% get back to normal. Age matters. If you’re over 65, your recovery rate drops by 35%. If your kidneys were already weak before AKI, your chance of full recovery is half.
Dialysis? Only 25% of patients who need it for AKI ever get off it completely. The rest develop chronic kidney disease.
And here’s the hidden cost: even if your creatinine returns to normal, you’re not back to normal. A 2022 survey of over 1,200 AKI survivors found 68% had “kidney fatigue”-a deep, unrelenting exhaustion that lasted 3-6 months. 42% had anxiety about their kidneys. 29% couldn’t return to work because they couldn’t walk more than 50 feet without stopping.

What Happens After You Leave the Hospital
AKI doesn’t end when you’re discharged. In fact, the real battle begins then.
23% of AKI survivors develop chronic kidney disease within a year. Each episode increases your risk of needing dialysis fivefold over the next five years.
That’s why follow-up is non-negotiable. You need a nephrologist visit within 6 months. Your creatinine, eGFR, and urine albumin must be tracked. Blood pressure and diabetes must be tightly controlled.
Avoid NSAIDs like ibuprofen. Watch your salt. Drink enough water, but don’t overdo it. Your kidneys are still healing.
Some patients never fully recover. But many do-especially if the cause was caught early. One man in Toronto had AKI from dehydration after a bout of food poisoning. His creatinine jumped to 1.8 (normal was 0.9). He got 2 liters of IV fluids in the ER. By the next day, it was back to 1.0. He went home in 24 hours. No dialysis. No long-term issues.
Another man, 72, had AKI from sepsis. He spent 17 days in the ICU on CRRT. His creatinine normalized after 3 weeks. But for 3 months, he could barely walk. He had panic attacks every time he felt tired. He needed counseling. He still checks his kidney numbers every 3 months.
The Future: Catching AKI Before It Starts
The next big leap isn’t better dialysis-it’s prevention.
AI algorithms are being trained to scan electronic health records and predict AKI 12-24 hours before it happens. By spotting patterns-like a drop in urine output, rising creatinine, or a new antibiotic-these systems can alert doctors before the damage is done.
A trial in Pittsburgh showed this approach reduced AKI incidence by 25% in high-risk patients.
Point-of-care urine tests for NGAL are now available in some Canadian hospitals. They cost $40 but can save thousands in ICU bills and prevent permanent damage.
The goal isn’t just to treat AKI. It’s to stop it before it begins.
What You Can Do Right Now
If you’re at risk-older, diabetic, on multiple meds, recently hospitalized-know the signs. If you feel unusually tired, swollen, or confused, get your creatinine checked. Don’t wait.
If you’re recovering from AKI, don’t assume you’re fine. Follow up. Track your numbers. Protect your kidneys like they’re your most important organ-because they are.
AKI doesn’t care if you’re healthy or sick. It strikes fast. But with awareness, early testing, and smart care, recovery isn’t just possible-it’s common.






Barry Sanders November 15, 2025
This is why I hate when people ignore 'routine blood work.' One day you're fine, next day you're on dialysis. No warning. No mercy. Just a number on a screen that says 'you're dying.'
Chris Ashley November 16, 2025
bro i had this last year after a bad flu. thought i was just tired. turned out my creatinine was 2.1. they gave me fluids and i was out in 36 hours. but man, the fatigue lasted 4 months. like, i couldn't walk to the fridge without needing a nap. no one talks about that part.
kshitij pandey November 17, 2025
In India, many people don't even know what kidneys do. I told my uncle he needs to check his creatinine after his fever - he said, 'It's just a cold, beta.' Now he's on dialysis twice a week. Please, if you're over 50 or on meds, get tested. It's cheap. It's easy. It saves your life.
Brittany C November 18, 2025
The biomarker data is compelling - NGAL and TIMP-2/IGFBP7 show promise in early detection, particularly in ICU settings where traditional markers lag. The temporal dissociation between tubular injury and serum creatinine elevation remains a critical diagnostic gap. Early intervention based on these biomarkers could reduce progression to CKD by up to 40% in high-risk cohorts.
Sean Evans November 19, 2025
I can't believe people still think 'just drink water' fixes everything. 🤦♂️ I work in an ER. I've seen 80-year-olds with sepsis and AKI because their family said 'he's just dehydrated' for 3 days. You don't 'hydrate your way out' of ATN from vancomycin. Stop being a hero. Go to the hospital before you're a statistic.
Anjan Patel November 20, 2025
You know what's worse than AKI? The fact that hospitals charge $20,000 for a 3-day stay while your insurance denies coverage because 'it wasn't severe enough.' I watched my neighbor die because he couldn't afford the dialysis. This isn't medicine - it's a lottery. And the poor always lose.
Scarlett Walker November 20, 2025
I had AKI after my C-section. No one warned me. I thought the swelling was normal. Turns out I had prerenal from blood loss. They gave me fluids, I bounced back, but I still get nervous every time I take ibuprofen. I'm so glad I found this post - I'm sending it to all my mom friends. We need to talk about this!
Hrudananda Rath November 21, 2025
It is, without a doubt, a matter of profound concern that the medical community continues to rely upon antiquated metrics such as serum creatinine - a biomarker with well-documented latency and insensitivity - for the diagnosis of a condition as dynamically pathophysiological as AKI. The absence of universal adoption of real-time, point-of-care biomarkers constitutes a systemic failure of clinical foresight, and indeed, a moral dereliction of duty.
Brian Bell November 21, 2025
I'm a nurse in Chicago. We started using NGAL tests last year. One guy? His creatinine was normal. NGAL spiked. We caught it. He didn't even need dialysis. It's wild how much this stuff changes outcomes. I wish everyone knew this. :)
Barry Sanders November 22, 2025
The author is right - recovery isn't guaranteed. But the real tragedy? The people who bounce back but can't work anymore. I'm one of them. I used to run marathons. Now I need a cane to walk to the mailbox. No one talks about the invisible damage.