Antipsychotic Medication Comparison Tool
Find the most suitable antipsychotic medication based on your specific symptoms, side effect concerns, and medical priorities. This tool analyzes your preferences against clinical data to show which medications best match your needs.
Select which symptoms are most prominent for you
Check all side effects you want to minimize
How important is medication cost to you?
Select your pregnancy status or considerations
Important: This tool is for informational purposes only. Always discuss medication decisions with your psychiatrist or healthcare provider. Do not change or stop medications without professional guidance.
Based on your selections, the following medications best match your needs:
How to use this information
This tool identifies medications that best align with your priorities based on clinical data. It does not replace professional medical advice. Always discuss these options with your psychiatrist to determine the right choice for your individual situation.
Consider sharing your results with your healthcare provider to have a more informed discussion about treatment options.
When you or a loved one is prescribed Amisulpride is a selective dopamine D2/D3 antagonist marketed under the brand name Solian. It’s primarily used for treating schizophrenia and, in some countries, depressive episodes. But how does it stack up against the other pills you might hear about at the doctor’s office? This guide walks through the most common alternatives, highlights key differences, and helps you decide which option fits your situation.
Why Amisulpride Matters
Amisulpride works by blocking dopamine receptors in the brain, especially the D2 and D3 subtypes. By reducing dopamine transmission, it eases positive symptoms of schizophrenia such as hallucinations and delusions while having a milder impact on negative symptoms like social withdrawal. Its relatively selective action means fewer motor side effects compared with older, broader‑acting antipsychotics.
When Doctors Choose Amisulpride
Typical scenarios include:
- First‑line treatment for acute psychotic episodes when patients are sensitive to extrapyramidal symptoms.
- Adjunct therapy for mood disorders in regions where it is approved for depressive episodes.
- Patients who have failed on other atypical antipsychotics but can tolerate dopamine‑blocking agents.
Standard dosing ranges from 400 mg to 1200 mg daily, split into two doses. The drug reaches steady‑state after about a week, and its half‑life is roughly 12 hours, allowing for twice‑daily dosing.
Core Alternatives to Consider
Below you’ll find the most frequently mentioned rivals, each with a short snapshot. The first mention of each drug includes micro‑data markup for easy knowledge‑graph extraction.
Risperidone is a broad‑spectrum atypical antipsychotic that blocks dopamine D2 and serotonin 5‑HT2A receptors. It’s approved for schizophrenia, bipolar mania, and irritability associated with autism.
Quetiapine is an atypical antipsychotic with strong antihistamine and α‑adrenergic blocking properties, used for schizophrenia, bipolar disorder, and major depressive disorder as an adjunct.
Aripiprazole is a dopamine‑partial agonist and serotonin antagonist, marketed for schizophrenia, bipolar I, and as an add‑on for depression.
Haloperidol is a first‑generation (typical) antipsychotic that strongly blocks D2 receptors, primarily used for acute psychosis and Tourette syndrome.
Olanzapine is an atypical antipsychotic with potent dopamine and serotonin antagonism, indicated for schizophrenia and bipolar disorder.
Schizophrenia is a chronic mental health condition characterized by delusions, hallucinations, disorganized thinking, and social withdrawal.
Bipolar disorder is a mood disorder featuring alternating periods of depression and mania, often requiring mood‑stabilizing antipsychotics.
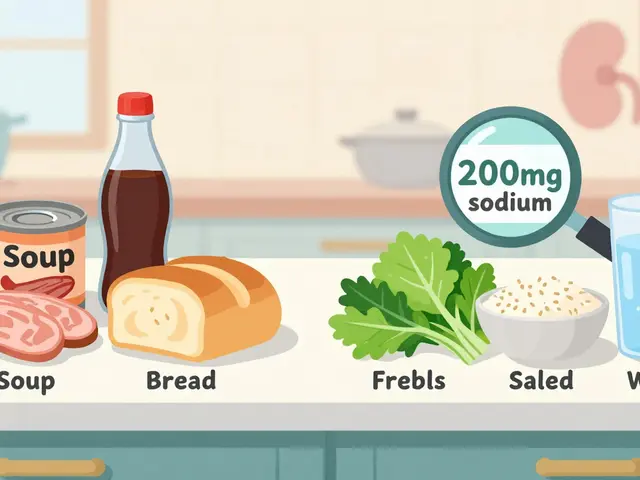
Side‑Effect Profiles at a Glance
Every antipsychotic carries a trade‑off. Understanding the most common adverse effects helps you weigh benefits against risks.
- Amisulpride: Usually mild weight gain, occasional prolactin elevation, low risk of metabolic syndrome.
- Risperidone: Prolactin increase, EPS (especially at doses >6 mg), moderate weight gain.
- Quetiapine: Sedation, orthostatic hypotension, significant weight gain, low EPS.
- Aripiprazole: Akathisia (restlessness), insomnia, minimal weight gain.
- Haloperidol: High EPS risk, tardive dyskinesia, low metabolic impact.
- Olanzapine: Marked weight gain, dyslipidemia, diabetes risk; low EPS.
Cost and Accessibility
Price varies by region and insurance coverage. In the United States, generic Amisulpride is not yet FDA‑approved, making it more expensive when imported. Risperidone and Quetiapine have widely available generics, often costing less than $30 per month. Aripiprazole and Olanzapine also have generics but can be pricier due to brand‑specific formulations. Haloperidol remains the cheapest typical antipsychotic, often under $10 per month.
Clinical Comparison Table
| Medication | Mechanism | Typical Daily Dose | Common Side Effects | FDA Approval Year (US) | Notable Advantage |
|---|---|---|---|---|---|
| Amisulpride (Solian) | D2/D3 selective antagonist | 400‑1200 mg (split BID) | Weight gain, prolactin rise | Not FDA‑approved (EU 1995) | Low metabolic impact, minimal EPS |
| Risperidone | D2 & 5‑HT2A antagonist | 2‑6 mg | Prolactin ↑, EPS, weight gain | 1993 | Effective for acute psychosis |
| Quetiapine | Multi‑receptor antagonist (D2, 5‑HT2A, H1) | 300‑800 mg | Sedation, hypotension, weight gain | 1997 | High tolerability, good for insomnia |
| Aripiprazole | D2 partial agonist, 5‑HT1A agonist | 10‑30 mg | Akathisia, insomnia | 2002 | Minimal weight gain, activating |
| Haloperidol | Strong D2 antagonist (typical) | 5‑20 mg | High EPS, tardive dyskinesia | 1958 | Low cost, rapid onset |
| Olanzapine | D2 & 5‑HT2A antagonist (atypical) | 10‑20 mg | Weight gain, metabolic syndrome | 1996 | Robust efficacy for both positive & negative symptoms |
Decision‑Making Checklist
Use this quick list when discussing options with your psychiatrist.
- Symptom profile: Dominant positive vs. negative symptoms.
- Metabolic concerns: Existing diabetes, BMI, cholesterol.
- Movement side‑effects: History of EPS or tardive dyskinesia.
- Sleep patterns: Need for sedation vs. need to stay alert.
- Cost & insurance: Generic availability, co‑pay.
- Pregnancy / lactation: Safety data for each drug.

Real‑World Scenarios
Case 1 - Young adult with first‑episode psychosis: The clinician wants a drug that controls hallucinations without putting the patient at high risk for weight gain. Amisulpride’s low metabolic footprint makes it a strong candidate, especially if the patient is already lean.
Case 2 - Middle‑aged patient with diabetes: Here, the priority is to avoid exacerbating glucose control. Aripiprazole’s minimal weight impact or Haloperidol (if EPS risk can be managed) would be preferred over Olanzapine or Quetiapine.
Case 3 - Patient struggling with severe insomnia: Quetiapine’s sedative effect can double as a sleep aid, but if daytime drowsiness is unacceptable, a low‑dose Atypical like Aripiprazole might be better.
How to Switch Safely
Changing antipsychotics isn’t a DIY task. Follow these steps:
- Talk to your prescriber about the reason for the switch.
- Start the new medication at a low dose while tapering the old one, unless a rapid cross‑taper is medically advised.
- Monitor for withdrawal symptoms (rebound psychosis, agitation) and emerging side effects.
- Schedule a follow‑up within 1‑2 weeks to adjust dosage based on response.
- Keep a symptom diary - note mood, sleep, appetite, and any movement changes.
Frequently Asked Questions
Is Amisulpride approved in the United States?
No. Amisulpride is licensed in many European countries and Canada, but it has not received FDA approval. Patients in the U.S. may obtain it through special import channels or clinical trials.
How quickly does Amisulpride start working?
Most patients notice a reduction in acute psychotic symptoms within 1‑2 weeks, though full effect on negative symptoms can take up to 6‑8 weeks.
Can I take Amisulpride with antidepressants?
Yes, many clinicians combine Amisulpride with SSRIs or SNRIs for mood‑disordered patients. However, watch for additive side effects such as increased prolactin.
What are the biggest risks of switching from Risperidone to Amisulpride?
Risperidone often causes higher prolactin levels; switching to Amisulpride might reduce that, but you could experience a brief rebound of psychosis if the cross‑taper isn’t gradual enough.
Is weight gain a concern with Amisulpride?
Weight gain is generally modest compared with Olanzapine or Quetiapine. Most studies report a mean increase of 1‑2 kg over six months.
Bottom Line
There’s no one‑size‑fits‑all answer. If metabolic health is a top priority and you need a drug with a clean EPS profile, Amisulpride (or its generic equivalents where available) stands out. For patients who value rapid symptom control and cost‑effectiveness, Haloperidol or generic Risperidone may be better. Always let a qualified psychiatrist weigh these factors against your personal medical history.





Hershel Lilly October 26, 2025
Amisulpride’s low‑impact metabolic profile makes it a solid pick when weight gain is a concern. Because it mainly targets D2/D3 receptors, it tends to spare the serotonin‑mediated appetite pathways that drive the heavier side‑effects of drugs like Olanzapine. The modest prolactin rise is something to monitor, but it’s generally easier to manage than the EPS risk you see with typical antipsychotics. In practice, many clinicians start with a split‑dose regimen of 400 mg BID and adjust based on symptom control and tolerability.
Monika Pardon October 28, 2025
Ah, the grand tapestry of pharmaceutical intrigue, where a Swiss‑made dopamine blocker somehow evades the mighty FDA. One might wonder whether the “import‑only” status is a clever ruse to keep us all in the dark about hidden side‑effects. Rest assured, the only conspiracy here is the industry’s love for exclusive pricing, not a covert brain‑washing agenda. Nevertheless, the data still show a relatively clean EPS record, even if the paperwork is scarce.
Jacqui Bryant October 31, 2025
Keep pushing forward, every small step toward the right med matters!
Manoj Kumar November 2, 2025
Choosing an antipsychotic is less about the molecule and more about the narrative we tell ourselves about control and freedom. If you value a drug that whispers rather than shouts at dopamine, Amisulpride fits that subtlety. Yet, the universe tends to reward those who weigh the whole picture-cost, side effects, and personal lifestyle. In the end, the best choice is the one that aligns with your own story, not just the latest headline. And if you happen to enjoy a little irony, remember that the “atypical” label is itself a philosophical joke about classification.
Carla Smalls November 4, 2025
It’s encouraging to see you weigh both the metabolic side‑effects and the movement risks; that balanced view often leads to a smoother transition when you switch meds. Staying informed about your own health numbers will make the conversation with your psychiatrist much more productive.
Rachel Zack November 7, 2025
Honestly, i think it’s a moral failur of the med industry to push pricier atypicals while ignoring the simple, effective options like amisulpride. Patients deserve transparency and not be forced into a cycle of ever‑increasing costs just to get decent care.
Johnae Council November 9, 2025
When evaluating Amisulpride against its peers, the first consideration should be the drug’s pharmacodynamic niche. By selectively antagonising D2 and D3 receptors, it avoids the broad serotonergic blockade that characterises many atypicals, which translates into a lower propensity for metabolic syndrome. Clinicians often appreciate this profile when treating patients who are already overweight or diabetic, as the weight‑gain risk is comparable to placebo in short‑term studies. On the other hand, the drug’s prolactin‑raising effect, while modest, can be clinically significant for individuals prone to galactorrhea or sexual dysfunction. The literature also suggests a dose‑dependent increase in prolactin, so staying at the lower end of the therapeutic window (around 400 mg BID) can mitigate this issue. From a movement‑disorder perspective, Amisulpride fares better than typical antipsychotics such as Haloperidol, which carry a high EPS burden, yet it is not entirely free of extrapyramidal symptoms at higher doses. This middle ground makes it a reasonable bridge for patients who have failed on more metabolically friendly agents like Aripiprazole but cannot tolerate the rigidity of Haloperidol. Economically, the lack of FDA approval in the United States inflates the cost, as patients must rely on importation or clinical trial enrollment, often leading to out‑of‑pocket expenses that can exceed $200 per month. In contrast, generics of Risperidone or Quetiapine are readily available for under $30, presenting a stark affordability gap. Insurance formularies typically favor FDA‑approved drugs, so prescribers may need to justify the clinical necessity of Amisulpride through prior‑authorization letters. The safety profile, while generally favourable, still warrants routine monitoring of prolactin levels, weight, and lipid panels, especially during the first six months of therapy. Switching from a drug like Risperidone requires a careful cross‑taper; abrupt discontinuation can precipitate rebound psychosis, whereas a gradual overlap helps maintain symptom control. Moreover, the half‑life of roughly 12 hours permits BID dosing, which some patients find more convenient than the nightly dosing required for Quetiapine’s sedative effect. Ultimately, the decision matrix should incorporate the patient’s metabolic status, history of EPS, cost considerations, and personal preference regarding dosing frequency. By weighing these factors systematically, clinicians can position Amisulpride as either a first‑line option for metabolically vulnerable patients or a strategic swap when other atypicals fall short.
Jennyfer Collin November 11, 2025
It is noteworthy that the regulatory pathways governing Amisulpride’s entry into the American market appear disproportionately opaque, raising legitimate concerns about the influence of multinational pharmaceutical lobbying on FDA decisions. The strict import restrictions, coupled with limited clinical trial data released to the public, create an environment where clinicians must rely on foreign literature that may not meet domestic evidentiary standards. Consequently, patients are left navigating a maze of off‑label prescriptions, insurance denials, and potential legal ramifications, all of which underscore a systemic bias towards domestically sanctioned compounds.
Brady Johnson November 13, 2025
Behind the veneer of “clinical necessity,” there lies a shadowy network of profit‑driven stakeholders who deliberately withhold affordable alternatives like Amisulpride to sustain their revenue streams. The timing of its delayed US approval aligns suspiciously with the launch of newer, costlier atypicals, suggesting a coordinated effort to monopolise the market. Patients who question this arrangement often find their concerns dismissed as “misinformation,” effectively silencing dissent and preserving the status quo.
Jay Campbell November 16, 2025
Sounds like you’ve got a solid plan-keep tracking those side‑effects and stay in close contact with your doctor.
Laura Hibbard November 18, 2025
Oh great, another medication choice to add to the list-just what we needed, right? But seriously, being proactive about the pros and cons will make the whole process feel a lot less like a guessing game.