Inflammation is a biological response that protects tissue from injury, infection, or irritants by recruiting immune cells and releasing signaling molecules. When the process becomes chronic, it can damage the very structures it aims to defend, especially in the mouth where bacteria, diet, and habits constantly challenge the tissues.
Why Inflammation Matters for Your Teeth and Gums
Every bite sends a tiny army of oral bacteria microorganisms that colonize the tooth surface and gums into contact with your enamel. A balanced oral microbiome the community of beneficial and harmful microbes living in the mouth keeps inflammation in check. When plaque builds up, harmful strains dominate, triggering the immune system to release cytokines protein messengers like IL‑1β, TNF‑α, and IL‑6 that amplify inflammation. Persistent cytokine release leads to the swelling, bleeding, and tissue breakdown that characterize gum disease.
Key Inflammatory Conditions in the Mouth
The two most common inflammation‑driven gum diseases are gingivitis a reversible inflammation of the gum margin caused by plaque buildup and periodontitis a chronic infection that destroys the supporting bone and connective tissue around teeth. Both start with plaque, but their outcomes differ dramatically.
| Feature | Gingivitis | Periodontitis |
|---|---|---|
| Primary tissue affected | Gum margin (gingiva) | Supporting bone & periodontal ligament |
| Reversibility | Yes - with proper cleaning | Limited - may need surgery |
| Typical symptoms | Redness, swelling, bleeding on probing | Pocket formation, bone loss, tooth mobility |
| Key cytokines | IL‑1β, TNF‑α (moderate levels) | IL‑1β, TNF‑α, IL‑6 (high levels) |
| Systemic links | Rare | Strong - cardiovascular, diabetes risk |
Notice how cytokine intensity rises from gingivitis to periodontitis, and how the disease starts to influence systemic health once bone loss begins.
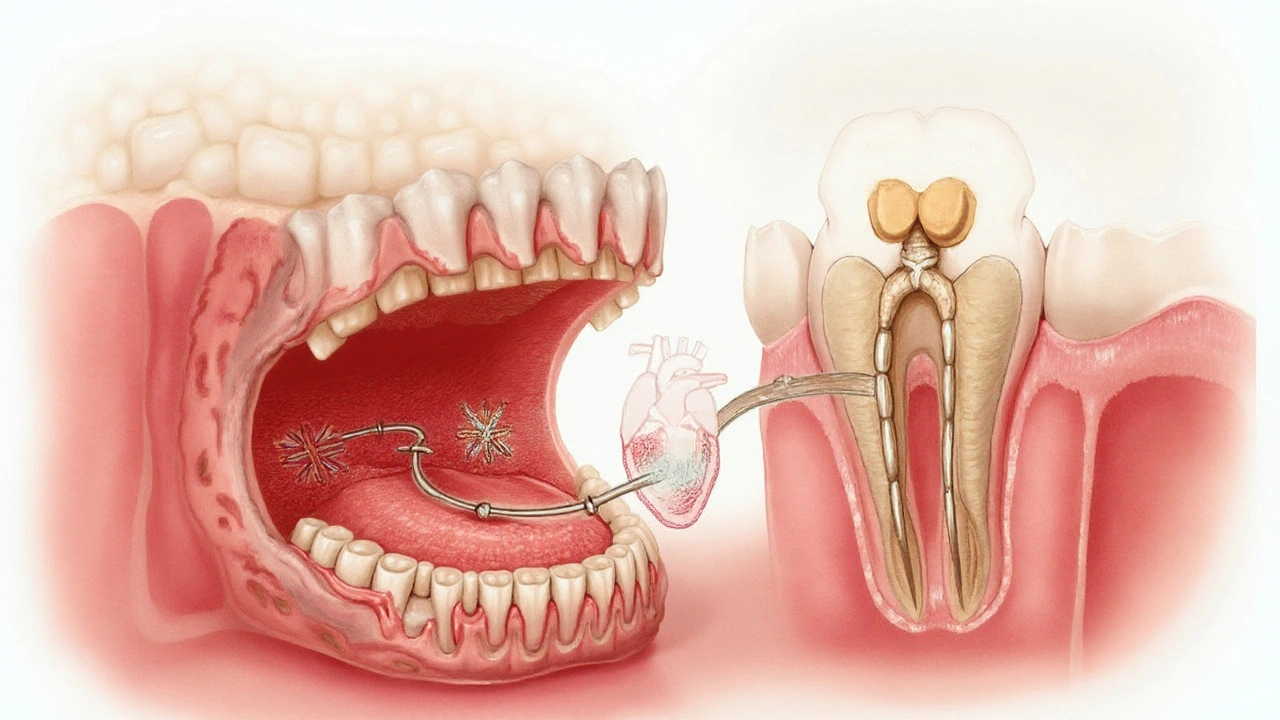
How Oral Inflammation Connects to Whole‑Body Health
Researchers repeatedly find that chronic gum inflammation is a red flag for systemic diseases conditions that affect the entire body, such as heart disease, stroke, and rheumatoid arthritis. The proposed mechanisms involve bacteria‑laden blood clots and the spillover of pro‑inflammatory cytokines into circulation. For instance, people with uncontrolled diabetes a metabolic disorder that impairs blood sugar regulation are twice as likely to develop severe periodontitis because high glucose fuels bacterial growth and weakens immune response.
Another notorious partner is smoking the inhalation of tobacco smoke, which compromises blood flow and immune function. Smokers often exhibit deeper periodontal pockets and slower healing after dental procedures, underscoring the synergy between toxin‑induced inflammation and bacterial aggression.
Risk Factors That Fuel Oral Inflammation
- Plaque accumulation: The primary driver; biofilm harbors pathogenic bacteria.
- Inadequate oral hygiene daily brushing and flossing routines: Missed cleaning leaves food particles for microbes.
- High‑sugar diet: Feeds bacteria, spikes insulin, and raises cytokine levels.
- Hormonal changes fluctuations during pregnancy, menopause, or puberty: Increase gum sensitivity to plaque.
- Genetic predisposition: Certain gene variants affect cytokine production, making some people more prone to aggressive periodontitis.
Each factor interacts with the others, creating a feedback loop where inflammation fuels more bacterial growth, which in turn fuels more inflammation.
Practical Ways to Tame Inflammation and Protect Your Smile
- Brush twice daily with fluoride toothpaste. Use a soft‑bristled brush and spend at least two minutes covering all surfaces.
- Floss or use interdental cleaners every night to disrupt plaque below the gum line.
- Schedule professional cleanings every six months; a dental hygienist can remove tartar that brushes miss.
- Adopt an anti‑inflammatory diet: foods rich in omega‑3 fatty acids nutrients found in fatty fish, flaxseed, and walnuts that dampen cytokine production and antioxidants like berries, leafy greens, and green tea.
- Quit smoking or use cessation aids; the reduction in toxin‑induced inflammation quickly improves gum healing.
- Manage systemic conditions: tight blood‑sugar control in diabetes and regular cardiovascular check‑ups lower the overall inflammatory load.
- Consider targeted anti‑inflammatory agents: short courses of NSAIDs non‑steroidal anti‑inflammatory drugs like ibuprofen that temporarily lower prostaglandin levels can alleviate acute pain, but long‑term use should be guided by a dentist or physician.
- Explore natural adjuncts: curcumin mouth rinses, aloe‑vera gels, and probiotic lozenges have shown modest reductions in gingival inflammation in clinical trials.
Consistency is key. Even small daily habits create a hostile environment for harmful bacteria, keeping cytokine storms at bay.
Emerging Research: From Biomarkers to Personalized Care
Scientists are now measuring specific salivary biomarkers molecular indicators like MMP‑8, IL‑1β, and CRP that reflect tissue inflammation to predict disease progression before clinical signs appear. In the next few years, a simple at‑home test could alert you to rising inflammatory markers, prompting early professional intervention.
Another frontier is personalized dentistry via genetic profiling. Certain alleles linked to aggressive periodontitis (e.g., IL‑1 genotype) may guide clinicians to more aggressive preventive regimens for at‑risk patients.
Connecting the Dots: Related Concepts Worth Exploring
Understanding oral inflammation opens doors to several adjacent topics:
- periodontal regeneration advanced surgical techniques that rebuild lost bone and ligament
- oral microbiome modulation using pre‑biotics, probiotics, or targeted antimicrobial peptides to restore a healthy bacterial balance
- systemic inflammation monitoring tracking blood markers like C‑reactive protein to gauge overall health impact of gum disease
Each of these areas builds on the central premise that controlling inflammation in the mouth reverberates throughout the body.
Frequently Asked Questions
Can occasional gum bleeding be normal?
Mild bleeding after flossing or brushing often indicates early inflammation (gingivitis). If it persists for more than a week despite proper oral hygiene, it’s a sign to see a dentist.
How fast can gum disease progress from gingivitis to periodontitis?
The timeline varies. In aggressive cases, bone loss can begin within months of untreated gingivitis, especially in smokers or diabetics. Most people see a slower progression over several years.
Do anti‑inflammatory foods really help my gums?
Yes. Studies show that diets rich in omega‑3s, antioxidants, and low in refined sugars can lower salivary cytokine levels, reducing gingival inflammation.
Is there a link between gum disease and heart attacks?
Strong epidemiological evidence links chronic periodontitis with higher risk of cardiovascular events. The proposed pathway involves systemic spread of oral bacteria and inflammatory mediators that accelerate arterial plaque formation.
Can over‑the‑counter mouthwashes replace regular brushing?
Mouthwashes can reduce bacterial load temporarily, but they don’t remove plaque mechanically. Brushing and flossing remain essential for controlling inflammation.
What are the best signs that I need a professional cleaning?
Red, swollen gums, persistent bad breath, gum recession, or any tooth sensitivity after eating cold/hot foods should prompt a visit. Early intervention stops inflammation from becoming destructive.







Sadie Viner September 25, 2025
Inflammation may sound like a distant scientific term, but its impact on your smile is strikingly personal. When plaque lingers, the immune system unleashes cytokines that swell gums, bleed, and eventually erode bone. Maintaining a diligent twice‑daily brushing routine, complemented by nightly floss, can keep this cascade at bay. Think of oral care as a daily diplomatic treaty between your teeth and your body, one that demands respect and consistency.
Kristen Moss September 26, 2025
Yo, we Americans love our grill, so quit neglecting it. If you skip floss just because it’s “too much hassle,” you’re basically signing a treaty with gum disease. Grab that floss, brush like a champ, and show those bacteria who’s boss.
Rachael Tanner September 27, 2025
The oral microbiome resembles a nuanced tableau, where beneficial and mischievous microbes dance in delicate equilibrium. When plaque tilts the scale, pro‑inflammatory cytokines such as IL‑1β and TNF‑α crescendo, orchestrating tissue distress. A diet modest in refined sugars and generous in omega‑3s can subtly rebalance this microbial ballet, preserving gingival serenity.
Debra Laurence-Perras September 29, 2025
Remember, each small habit builds a fortress against inflammation. Regular professional cleanings act like a skilled siege engine, dismantling tartar that your toothbrush can't reach. By staying optimistic and consistent, you empower your gums to heal swiftly and stay resilient.
dAISY foto September 30, 2025
Yo, listen up-your mouth is a tiny universe, and every bite sends ripples through it!
Don't let the sugar monsters win; swap that soda for some green tea and feel the calm wash over your gums.
Stay fierce, stay fresh, and let that fresh breath be your battle cry!
We got this, fam, keep the flame of health burning bright!
Ian Howard October 1, 2025
Here’s a pragmatic yet dramatic rundown: brush twice a day with fluoride toothpaste, floss nightly, and schedule cleanings every six months. Sprinkle in anti‑inflammatory foods-think wild salmon, walnuts, and vibrant berries-to dampen cytokine storms. And remember, a short course of ibuprofen can tame acute pain, but don’t let it become a crutch without professional guidance.
Chelsea Wilmer October 2, 2025
When we contemplate the cascade of events that begins with a seemingly innocuous film of plaque, we are forced to acknowledge the intricate choreography of microbial invasion, immune activation, and tissue remodeling that follows. The first act, dominated by Streptococcus mutans and other early colonizers, sets the stage for a dysbiotic shift that amplifies the production of interleukin‑1β, tumor necrosis factor‑α, and interleukin‑6, each acting as a molecular siren calling forth inflammatory cells to the gingival frontier. As neutrophils swarm, they release proteolytic enzymes and reactive oxygen species, which, while intended to eradicate pathogens, inadvertently degrade collagen fibers and compromise the structural integrity of the periodontal ligament. This biochemical artillery, when unchecked, creates periodontal pockets that serve as reservoirs for anaerobic bacteria such as Porphyromonas gingivalis, further fueling a vicious feedback loop of cytokine release and connective tissue breakdown. The systemic ramifications of this local turmoil are profound; circulating inflammatory mediators can destabilize atherosclerotic plaques, thereby increasing the risk of myocardial infarction in susceptible individuals. Moreover, the chronic low‑grade inflammation associated with periodontitis can exacerbate insulin resistance, creating a bidirectional relationship with type 2 diabetes that complicates disease management. Smoking, with its vasoconstrictive and immunosuppressive qualities, amplifies these processes by impairing fibroblast function and reducing gingival blood flow, leading to deeper pockets and slower post‑procedural healing. Dietary patterns rich in refined sugars act as fertile ground for pathogenic biofilms, whereas omega‑3 fatty acids and polyphenols, abundant in fatty fish, flaxseed, and berries, can attenuate the inflammatory cascade by modulating eicosanoid pathways. Genetic predisposition, exemplified by polymorphisms in the IL‑1 gene cluster, predisposes certain individuals to heightened cytokine responses, rendering them more vulnerable to aggressive periodontitis even with modest plaque accumulation. In clinical practice, the integration of salivary biomarker analysis-measuring levels of matrix metalloproteinase‑8, C‑reactive protein, and interleukins-offers a promising avenue for early detection before overt clinical signs manifest. Emerging point‑of‑care technologies may soon empower patients to monitor these biomarkers at home, prompting timely professional intervention. Prophylactic measures, such as the routine use of antimicrobial mouth rinses containing chlorhexidine or essential oil blends, can reduce microbial load, yet they should complement-not replace-mechanical plaque removal. Patient education, delivered with empathy and cultural sensitivity, remains the cornerstone of sustained oral health, encouraging adherence to daily brushing, flossing, and regular dental visits. Ultimately, the battle against oral inflammation is won through a multifaceted strategy that intertwines meticulous hygiene, nutritional wisdom, lifestyle modification, and, when necessary, targeted pharmacologic therapy. By embracing this holistic approach, we not only preserve the integrity of our teeth and gums but also safeguard the broader tapestry of systemic well‑being.
David Stout October 3, 2025
Great points! Adding a quick tip: swapping out a regular mouthwash for one with xylitol can further inhibit plaque formation without the harsh alcohol burn.
Pooja Arya October 4, 2025
It is incumbent upon each of us to recognize that neglecting our oral health is not merely a personal failing but a societal sin that erodes the very foundation of communal well‑being. When we indulge in sugary indulgences without restraint, we betray the trust our bodies place in us, inviting inflammation that ripples beyond the gums to jeopardize hearts and souls alike. Let us therefore pledge to honor our bodies with disciplined hygiene, mindful nutrition, and reverence for the intricate ecosystems residing within our mouths.
Sam Franza October 6, 2025
Floss daily it works.
Raja Asif October 7, 2025
Our nation’s strength lies in disciplined citizens who protect every part of their health, including the gums; weak oral care is a betrayal of national pride.
Matthew Tedder October 8, 2025
Remember that consistent, gentle care is the most compassionate approach you can take for your own body, and it sets a calming example for those around you.
Cynthia Sanford October 9, 2025
Yo, keep that vibe rollin-if u floss everyday u’ll be smilin bright all day!
Yassin Hammachi October 10, 2025
In the grand tapestry of health, oral inflammation is a single thread that, when tugged, can alter the pattern of the whole fabric; tending to it with mindful routine weaves resilience throughout our lives.