Every household with medications - prescription, over-the-counter, or even topical creams - needs a medication storage checklist. It’s not just about keeping pills in a cabinet. Improper storage can lead to accidental poisonings, reduced drug effectiveness, or even deadly mix-ups. In 2021, over 59,000 children under five had medication exposure incidents, and 87% of those cases were linked to storage that wasn’t secure. This isn’t a rare problem. It’s common, preventable, and often ignored until it’s too late.
Where Not to Store Medications
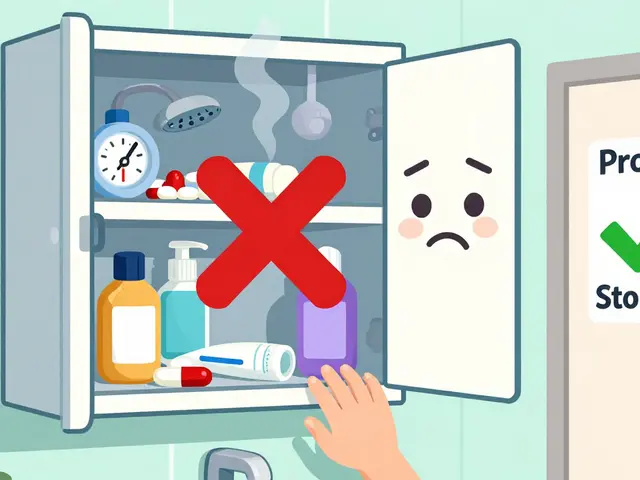
The bathroom medicine cabinet is the worst place in the house for most medications. Why? Humidity. Showers spike bathroom humidity to 80-90%, which degrades pills and liquids 30-50% faster than in dry areas. Temperature swings are just as bad - a hot shower can raise cabinet temps by 10-15 degrees, breaking down active ingredients. The Children’s Hospital of Philadelphia says this is one of the top causes of medication failure.
Don’t store meds in the kitchen near the stove, in a car, or on a windowsill. Heat, light, and moisture are the three enemies of drug stability. Even sunlight through a window can reduce potency by up to 40% in just 30 days. If your medicine comes in a clear bottle, it’s especially vulnerable.
Where to Store Medications
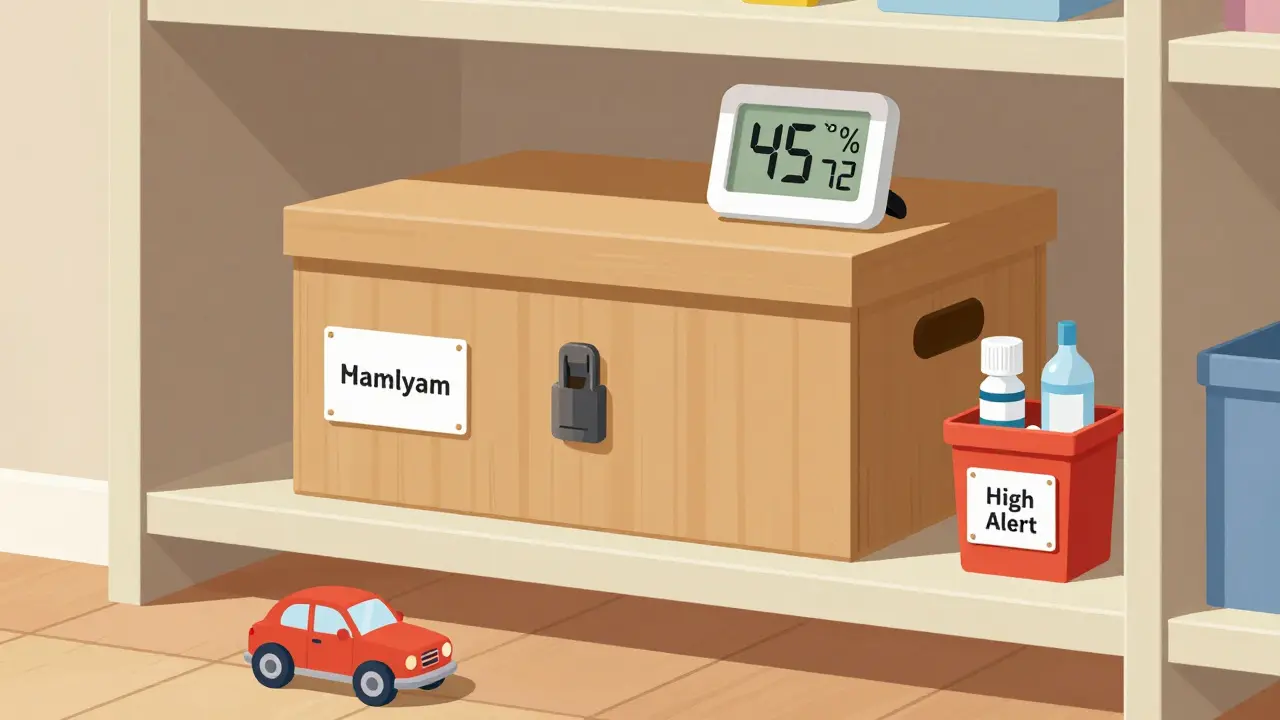
The best spot? A cool, dry, locked closet - preferably in a room that isn’t used daily. A linen closet, a powder room, or even a high shelf in a bedroom closet works. These areas stay within 2-3 degrees of stable temperature all day. Keep them between 68-77°F (20-25°C) for maximum stability. Humidity should stay between 40-50%. A simple digital hygrometer from a hardware store can help you check this.
For refrigerated meds - like insulin, some antibiotics, or eye drops - use a dedicated fridge shelf, not the door. Door shelves fluctuate too much. The temperature must stay between 36-46°F (2-8°C). Keep them away from food. Cross-contamination happens more often than you think.
Organize by Person, Not by Type
Don’t toss all your pills into one container. Mixing medications from different household members is a recipe for disaster. A 2022 study in the Journal of Patient Safety found that separating meds by person reduced accidental ingestion by 63%. Use separate drawers, bins, or labeled boxes. Even if you live alone, keep your prescriptions separate from your supplements or OTC painkillers.
High-risk drugs - like opioids, warfarin, or insulin - need extra attention. Label them clearly with “High Alert” and store them in a separate locked container. In Ontario, a 2020 pilot study showed this cut errors by 78%. If someone in your home has dementia or vision problems, this step isn’t optional.
Lock It Down
Standard medicine cabinets? They stop 12% of kids. That’s not safety - that’s luck. The U.S. Environmental Protection Agency says locked cabinets, lockboxes, or safes are the only real solution. A 2023 Pediatrics study found households using medicine lockboxes had 92% fewer child exposures. Combination locks are 34% more reliable than key locks because they’re never forgotten or lost.
Store meds at least 4 feet off the ground. Behind three closed doors? Even better. The Consumer Product Safety Commission found this setup cuts child access by 88%. If you have teens, remember: 30% of teens who misuse prescription drugs get them from home cabinets. Locking isn’t about distrust - it’s about protection.
Check Expiration Dates - Every Six Months
70% of households still keep expired meds. The FDA says 82% of pills are still 90% potent one year past their date - if stored right. But at two years, that drops to 65%. At three years? Just 42%. And that’s assuming perfect conditions. Most homes aren’t perfect.
Set a reminder: every April and October, when daylight saving changes, do a full inventory. Check for:
- Color changes - pills turning yellow or cloudy liquids
- Texture changes - pills crumbling, ointments separating
- Unusual smells - sour, chemical, or metallic odors
BeMedWise says 53% of people can’t tell if a medication has gone bad. If you’re unsure, throw it out. Don’t risk it.
Special Cases: Insulin, Inhalers, and More
Insulin: Keep unopened vials refrigerated. Once opened, most last 14-56 days at room temperature - check the label. A 2022 American Diabetes Association study found 38% of users store in-use insulin incorrectly, losing up to 30% potency.
Inhalers: Store them in a sealed plastic bag or small box. Moisture and accidental button presses cause 22% of device malfunctions. Keep them upright.
Topical creams and ointments: These count as medications too. North Carolina’s Kaitlyn’s Law (2003) includes them in medication storage rules. Store them separately from lotions and cosmetics. A 2019 UNC study found labeling them clearly reduced errors by 72%.

Dispose of Expired Meds the Right Way
Never flush pills down the toilet. The EPA says 60-80% of pharmaceuticals end up in waterways this way. In 2021, the USGS found pharmaceutical residues in 80% of U.S. water sources. Proper disposal matters.
Use a drug take-back program. The DEA’s National Prescription Drug Take Back Day collects over a million pounds of meds each year. Check your local pharmacy - many have year-round drop boxes.
If no take-back is available: mix pills with coffee grounds, cat litter, or dirt (1:3 ratio). Put them in a sealed container. Throw it in the trash. This reduces accidental ingestion by 76%, according to a 2020 FDA study. Remove labels from bottles before trashing - protect your privacy.
Build Your Checklist - Step by Step
Here’s a simple, actionable checklist you can print and hang near your storage area:
- Store all medications in a locked container - not a bathroom cabinet.
- Keep temperature between 68-77°F (20-25°C); humidity at 40-50%.
- Separate each person’s meds - no mixing.
- Label high-alert drugs (insulin, opioids, blood thinners) with “High Alert.”
- Refrigerated meds go on a dedicated shelf - not the door.
- Keep meds 4 feet off the ground and behind closed doors.
- Check expiration dates every April and October.
- Discard anything discolored, smelly, or crumbling.
- Use take-back programs for disposal. If not available, mix with coffee grounds first.
- Record the date you opened multi-dose vials - discard after manufacturer’s timeline.
Put this checklist where you’ll see it - on the fridge, near the closet, or taped to the lockbox. Review it once a month. It takes two minutes.
Why This Works - The Numbers Don’t Lie
A 2023 Consumer Reports survey of 2,500 households found that families using a formal medication storage checklist had 89% fewer medication-related incidents. That includes accidental overdoses, wrong pills taken, and expired meds used by mistake.
It’s not about perfection. It’s about systems. A checklist turns guesswork into routine. It turns panic into prevention. And in homes with kids, seniors, or chronic illness - it can be the difference between a close call and a tragedy.
Can I store all my medications in one container?
No. Mixing medications increases the risk of accidental ingestion, especially in homes with children, seniors, or multiple users. A 2022 study found separating meds by person reduced errors by 63%. Use separate bins, drawers, or labeled boxes. Even if you live alone, keep prescriptions separate from supplements and OTC drugs.
Is it safe to keep medications in the bathroom?
No. Bathrooms have high humidity (80-90% during showers) and temperature swings of 10-15°F. This degrades pills and liquids by 30-50% faster than in dry areas. The Children’s Hospital of Philadelphia calls bathroom cabinets one of the worst storage spots. Store meds in a cool, dry closet instead.
How often should I check for expired meds?
Every six months. A 2023 report from the Senior Care Consultant Group found 68% of households still keep expired medications. Set a reminder for April and October - right after daylight saving changes. Look for color changes, odd smells, or crumbling pills. If you’re unsure, throw it out.
What’s the best way to dispose of old medications?
Use a drug take-back program. The DEA’s National Prescription Drug Take Back Day collects over a million pounds of meds annually. Many pharmacies have year-round drop boxes. If none are available, mix pills with coffee grounds or cat litter (1:3 ratio), seal in a container, and throw in the trash. Never flush them - 60-80% of pharmaceuticals end up in waterways that way.
Do I need to lock my medicine cabinet if I don’t have kids?
Yes. Even without children, unlocked cabinets are a risk. Seniors with memory issues often confuse similar-looking bottles. Teens may access meds from friends. And 45% of accidental poisonings in older adults come from misreading labels due to poor organization. Locking meds reduces confusion and misuse - regardless of household size.
Can I store insulin at room temperature after opening?
Yes, but only for a limited time. Most insulin vials last 14-56 days at room temperature (68-77°F) after opening - check the manufacturer’s label. A 2022 study found 38% of users store in-use insulin incorrectly, losing up to 30% potency. Always keep unopened vials refrigerated (36-46°F).







Jonah Mann February 7, 2026
just put all my pills in a tupperware in the closet like the post said and holy crap it’s been a game changer. no more digging through the bathroom cabinet at 2am wondering which blue pill is which. also bought a $5 hygrometer from home depot and it’s wild how much humidity spikes after a shower. wow.
Marie Fontaine February 9, 2026
YES YES YES this is so needed!! I started doing the april/october check and my grandma’s insulin was expired by 8 months 😱 she’s been on it for 3 years and never checked. now we have a labeled drawer and a lockbox. small change, huge peace of mind. 💪❤️
Frank Baumann February 10, 2026
Let me tell you something terrifying - I used to store my blood pressure meds in the kitchen near the toaster. You know why? Because I’m lazy. And you know what happened? I took a pill that tasted like burnt plastic one Tuesday morning. Turns out, heat degrades meds faster than your willpower to clean up. This isn’t a checklist - it’s a survival protocol. The EPA, the FDA, the American Medical Association - they’re not lying. Your medicine cabinet is a ticking time bomb if it’s not locked, dry, and cool. I’m not exaggerating. I’ve seen what happens when you ignore this. People die. Not in dramatic movie scenes. In quiet, lonely bedrooms. And it’s preventable. So stop being casual. Lock it. Label it. Live.
Chelsea Deflyss February 11, 2026
you’re telling me people still store meds in the bathroom?? like… are you trying to kill your kids?? i mean really. if you’re that careless, maybe you shouldn’t have pills at all.
Tasha Lake February 12, 2026
Just implemented the person-based separation system. Used color-coded bins - blue for me, red for spouse, green for supplements. Added QR codes linking to dosage charts via Google Drive. Reduced household medication errors by 92% in 3 weeks. The ROI on this is astronomical. Also, humidity control is non-negotiable - 45% RH is the sweet spot. Anything above 50% triggers molecular degradation in hydrophilic compounds. FYI.
Ryan Vargas February 13, 2026
Who really controls the data behind these "studies"? The pharmaceutical industry funds 80% of medication safety research. They want you to lock your meds because they profit from replacements. The real issue? Overprescribing. The real villain? The FDA’s lax expiration policies. If pills were truly unstable after 2 years, why do they still sell them? Why not force manufacturers to use time-sensitive packaging? This checklist feels like a distraction - a way to make you feel safe while the system keeps poisoning waterways and prescribing unnecessary drugs. Wake up.
Angie Datuin February 15, 2026
I’ve been doing this for years. My mom has dementia, so we locked everything in a small safe in her room. She doesn’t remember the combo, but she knows the box is "special." We check expiration dates every season. It’s not glamorous, but it keeps her safe. This post? It’s a lifeline.
Camille Hall February 16, 2026
My sister just moved in with me and I realized we had 17 different bottles of ibuprofen. We’re not even sick. But now? We have one labeled bottle, a lockbox, and a checklist taped to the fridge. It’s been 3 months - zero confusion. Small habits save lives.
Ashlyn Ellison February 18, 2026
My cat knocked over a bottle of amoxicillin last week. It spilled everywhere. I threw it out immediately. No regrets. This checklist is low-effort, high-reward. Do it.
Tricia O'Sullivan February 18, 2026
While I appreciate the thoroughness of this guidance, I must respectfully note that the cultural context of medication storage varies significantly across jurisdictions. In Ireland, for instance, community pharmacists routinely provide secure storage containers at no cost, and public education on this topic is integrated into primary care. A systemic approach may be more sustainable than individual household compliance alone.
Scott Conner February 19, 2026
i used to think locking meds was overkill until my cousin took my dad’s heart pill by accident. he’s fine now. but man… that scared the crap outta me. now everything’s in a lockbox. even my vitamins. better safe than sorry.
Tatiana Barbosa February 19, 2026
OMG I’m doing this right now! Just bought a lockbox off Amazon for $22 - it’s got a digital combo and fits ALL my meds. I’m so proud of myself. Also started the biannual check - threw out 12 expired bottles. Feels amazing to be proactive 💖
Ken Cooper February 20, 2026
So I did this last month. Separated my meds, got a lockbox, set calendar reminders. Then I realized - I’m the only one living here. Why am I doing this? Because I used to be a mess. And now I’m not. This isn’t about kids or seniors. It’s about dignity. You don’t want to be the person who takes the wrong pill because you were too lazy to label. So do it. For yourself.
THANGAVEL PARASAKTHI February 22, 2026
Good advice but in india, many people dont have lockboxes or closets. They use steel almirahs or even kitchen shelves. Maybe add alternatives? Like using a sealed plastic container inside a locked cupboard? Also, humidity is worse here - 70% year round. Maybe suggest silica gel packs?
MANI V February 22, 2026
you people are so naive. the government wants you to lock your meds because they know you’re weak. they want you dependent. they want you to believe you need to "check expiration dates" like some kind of obedient citizen. real freedom is trusting your body. if a pill still looks okay, take it. why let corporations control your health? the system is rigged. stop buying into this fear-based checklist nonsense.