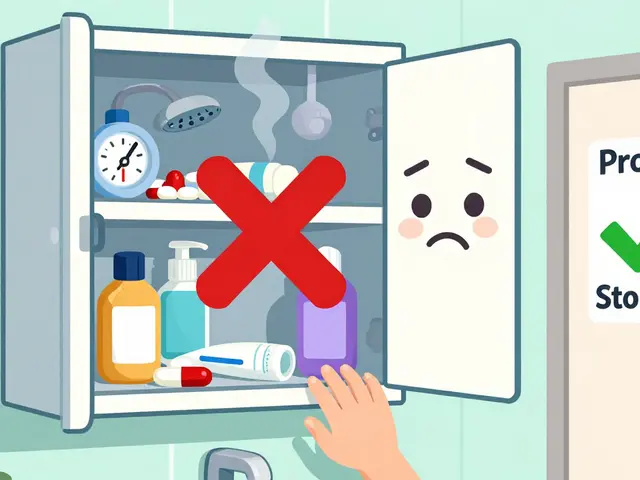
Most people keep their medications in the bathroom. It’s convenient - right next to the sink, easy to reach after brushing your teeth. But here’s the truth: storing medications in the bathroom is one of the most common and dangerous mistakes you can make with your prescriptions.
The bathroom isn’t just damp. It’s a chemical storm. Every time you take a hot shower, steam fills the air. Humidity spikes to 80-100%. Temperature jumps 20-30°F in minutes. That’s not just uncomfortable - it’s destroying your pills, patches, and liquids before you even take them.
Medications aren’t like socks or toothpaste. They’re complex chemical compounds designed to stay stable under specific conditions. Most require a cool, dry environment between 59°F and 77°F (15°C-25°C). Your bathroom? It rarely hits that range. And when it doesn’t, your drugs start breaking down.
How Heat and Moisture Destroy Your Medications
Water doesn’t just make your pills soggy - it chemically breaks them apart. Tablets absorb moisture, triggering a process called hydrolysis. That means the active ingredient - the part that actually treats your condition - starts falling apart. Capsules get sticky or brittle. Powders clump. Even liquid medications can separate or grow bacteria.
Some drugs are especially sensitive. Insulin? It’s a protein. Once it hits 86°F (30°C), it starts losing effectiveness. If you’re diabetic and your insulin has been sitting in a steamy cabinet for months, your blood sugar could spike without warning.
Nitroglycerin - the little tablet you take during a heart attack - loses potency within weeks if exposed to humidity. A study in Circulation found that patients storing beta-blockers in the bathroom had inconsistent blood pressure control 30.2% of the time. That’s not a small risk. That’s life-threatening.
Birth control pills? The FDA tested them. Humidity can reduce their effectiveness by up to 35%. That’s not a typo. That’s enough to cause an unintended pregnancy.
And it’s not just pills. Blood glucose test strips - used by millions - give false readings 68% of the time when stored in humid environments. If you’re managing diabetes, that means you could be making dangerous decisions based on wrong numbers.
Why Your Medicine Cabinet Is a Safety Hazard
It’s not just about potency. It’s about access.
Most bathroom cabinets aren’t locked. Kids climb on counters. Teens rummage through drawers. Pets jump up. The CDC says 70% of misused prescription opioids come from home medicine cabinets - and the bathroom is the #1 spot people keep them.
According to a NIH-funded study of 220 U.S. households, 80% of families stored medications in easily accessible places like the bathroom. Of those with children, 63% kept high-risk drugs within reach. The American Academy of Pediatrics says all medications should be locked away. Most homes? They’re failing.
And then there’s the quiet danger: antibiotics. If they degrade from moisture or heat, they don’t work as well. That means infections don’t clear up. Bacteria survive. And that’s how antibiotic resistance grows - one degraded pill at a time. The WHO calls this a global crisis. Your bathroom cabinet? It’s part of the problem.

Real Consequences: Stories Behind the Data
It’s not theoretical. People get hurt.
WELLFOR’s 2023 analysis found cases where degraded warfarin - a blood thinner - led to dangerous clots because the drug lost potency. Patients thought they were protected. They weren’t.
In London, Great Ormond Street Hospital reviewed pediatric medication errors and found that 4.3% were tied to expired or degraded drugs stored in bathrooms. One child got a weaker dose of an asthma inhaler. Another didn’t respond to antibiotics because they’d been sitting in steam for months.
On Reddit’s r/pharmacy, a March 2023 thread titled “Bathroom medicine cabinet ruined my blood pressure medication” had 87 comments. People described symptoms returning after refills. One nurse shared that 42% of patients’ medications showed visible signs of damage - crumbling, discoloration, stickiness - when stored in bathrooms. Only 8% showed damage when stored properly.
These aren’t outliers. They’re predictable outcomes of ignoring basic science.
Where You Should Store Medications Instead
The solution isn’t complicated. It’s simple.
Look for a cool, dry, dark place. Not near the stove. Not on the windowsill. Not in the car. Those spots get hot too.
The best spot? A bedroom dresser drawer. An interior closet. A shelf in your hallway. Anywhere with stable temperature - ideally varying by only 2-3°F daily, not 15-20°F like in the bathroom.
Use an airtight container if you want extra protection. Some pharmacies now include desiccant packets in bottles - little packets that soak up moisture. If yours doesn’t, you can buy them online for under $5.
For medications that need refrigeration - about 12% of prescriptions, like insulin or some eye drops - keep them in the fridge, but not in the door. The door opens and closes. That causes temperature swings. Put them in the back, where it’s coldest and most stable. And never store them in the kitchen fridge if you’re sharing it with food - cross-contamination is a real risk.

What to Do with Old or Expired Medications
If your meds have been sitting in the bathroom for years, they’re probably useless. Maybe even dangerous.
Don’t flush them. Don’t throw them in the trash. Don’t pour them down the sink. Those methods pollute waterways and harm wildlife. The EPA says 46% of medications found in rivers and lakes come from improper disposal.
Find a drug take-back program. Many pharmacies, hospitals, and police stations offer free drop-off bins. In Canada, pharmacies like Shoppers Drug Mart and Rexall have take-back programs. Check with your local pharmacy - they’re required to offer this service.
If no take-back option is available, mix pills with kitty litter, coffee grounds, or dirt. Put them in a sealed bag. Throw them in the trash. This makes them unappealing and unusable to kids or pets.
And clean out your cabinet every three months. That’s what hospitals recommend. If you can’t remember when you last refilled something, it’s probably expired.
What’s Changing - And What You Can Do Now
Pharmaceutical companies are finally waking up. Over 73% of prescription bottles now include storage instructions - up from 41% in 2015. Some labels even change color if exposed to heat or humidity.
Smart medicine cabinets are starting to appear - devices that monitor temperature and send alerts to your phone. But you don’t need tech to fix this. You just need awareness.
A 2023 study in the Journal of the American Pharmacists Association found that people who used medication apps with storage reminders improved their storage habits by 47%. That’s huge. A simple notification - “Check where your blood pressure meds are stored” - can save lives.
So here’s what to do today:
- Walk to your bathroom. Open the medicine cabinet.
- Take out every pill, bottle, and patch.
- Check expiration dates. Look for discoloration, crumbling, stickiness, or odd smells.
- Find a new home: a locked drawer in your bedroom, a closet shelf, a cabinet away from heat and moisture.
- Dispose of anything expired or damaged using a take-back program or safe disposal method.
- Set a reminder on your phone: “Check meds storage - every 3 months.”
This isn’t about being perfect. It’s about being safe. Your medications are your health. Don’t let your bathroom ruin them.
Can I store medications in the kitchen?
Only if it’s away from the stove, oven, or sink. Kitchens often get hot near appliances and humid near dishwashers. A cabinet far from the stove, like one in a pantry, is better than the bathroom - but still not ideal. A bedroom drawer is safer.
What if my medication says "store at room temperature"?
"Room temperature" means 59°F-77°F (15°C-25°C). That’s not your bathroom. That’s a closet in your bedroom or a drawer in your hallway. If your house gets hot in summer or cold in winter, those spots are still more stable than the bathroom.
Are over-the-counter meds safer to store in the bathroom?
No. Pain relievers, allergy meds, and cold pills degrade just like prescriptions. A 2021 study showed that antihistamines stored in humid environments lost potency fast - leading to failed allergy control. Don’t assume OTC means safe to store anywhere.
How do I know if my medication has gone bad?
Look for changes: pills that are crumbly, sticky, discolored, or smell odd. Liquids that are cloudy or have particles. Patches that are no longer sticky. If you’re unsure, don’t take it. Talk to your pharmacist - they can tell you if it’s still safe.
Is it okay to store medications in the car?
Never. Cars get extremely hot - over 140°F on a sunny day. That’s enough to melt pills, break down insulin, and ruin inhalers. Even in winter, freezing temperatures can damage some medications. Keep them in your home, not your vehicle.
What about medications that need refrigeration?
Keep them in the back of the fridge, not the door. The door opens often, causing temperature swings. Avoid storing them next to raw meat. Use a sealed container to prevent contamination. If you’re unsure, ask your pharmacist - some refrigerated meds need to be kept between 36°F and 46°F.
Can I trust the expiration date on the bottle?
Expiration dates are based on proper storage. If your meds were stored in a hot, humid bathroom, they may have degraded long before the date. If they look or smell off, discard them. Don’t wait for the date.









Janette Martens December 29, 2025
I keep my pills in the bathroom because my damn bathroom cabinet is the only one with a lock. My kid's a menace and my husband thinks Vicodin is candy. You think I wanna risk my meds in some drawer where the cat can knock 'em over? Fix the system, not the cabinet.
Marie-Pierre Gonzalez December 30, 2025
Thank you for this meticulously researched and profoundly important article. 🙏 The scientific rigor applied here is not merely commendable-it is essential for public health. I have already relocated all my medications to a locked, climate-controlled drawer in my bedroom. I urge everyone to do the same. Your life may depend on it. 💡
Louis Paré December 31, 2025
Let’s be real-this is just another wellness cult article dressed up as science. You know what’s *actually* dangerous? The pharmaceutical industry making you think your $150 insulin is going to turn into dust if you breathe near it. Most meds are fine. People are just scared of things they don’t understand. Also, your 'study' cited Reddit threads. That’s not evidence. That’s gossip.
Bradly Draper January 1, 2026
I never knew this. I kept my blood pressure pills in the bathroom for years. Now I feel kinda dumb. But I moved them to my nightstand and I feel way better about it. Thanks for the heads up.
Gran Badshah January 2, 2026
in india we keep medicine in bathroom because no one has drawers. and if you lock it then who will take it when grandma needs it at 3am? also bathroom is cool at night. your american fridge logic dont work here.
Ellen-Cathryn Nash January 2, 2026
I’m not saying you’re wrong… but I *am* saying you’re one of those people who treats their medicine like it’s a sacred relic. Meanwhile, I’ve got my aspirin in the bathroom and I’ve been fine for 20 years. Maybe your body’s just weak? Or maybe you’re just… overly dramatic? 😒
Samantha Hobbs January 4, 2026
I just moved all my meds to my bedroom drawer and now I’m obsessed. I labeled them with sticky notes. I even bought a little lockbox. I feel like a spy. But also, like a responsible adult. Who knew this was a thing??
Nicole Beasley January 5, 2026
OMG I had no idea 😱 I’ve been keeping my birth control in the bathroom since college. I just checked-my pills are kinda sticky. I’m throwing them out and getting a new pack. Thank you for saving me from a very bad situation 💕
sonam gupta January 6, 2026
you people worry too much. medicine lasts longer than you think. my mother kept everything in bathroom for 40 years. she lived to 92. your science is overrated
Julius Hader January 7, 2026
I used to think this was a myth too. Then my dad’s nitroglycerin didn’t work during his angina episode. Turns out it had been in the bathroom for 3 years. He’s fine now. But I’ll never forget that day. This isn’t hype. It’s survival.
Vu L January 8, 2026
What if I just don’t care? I’m not gonna rearrange my whole life because some guy with a PhD says my bathroom is a death trap. I’ve got a 5-year supply of ibuprofen in there and it’s been fine. Maybe your meds are just bad? Or maybe you’re just trying to sell a smart cabinet?
James Hilton January 9, 2026
Americans: turning medicine storage into a cult. Next you’ll be measuring humidity levels with a $200 app. Meanwhile, in Japan, they store everything in a cardboard box under the bed. They live longer. Maybe the real problem? You’re too anxious to be healthy.
Mimi Bos January 10, 2026
i moved my meds to the closet and now i keep forgetting they’re there. i took my blood pressure pill at 8pm last night and then again at 2am. oops. maybe the bathroom is better for me? at least i remember it there.