When you pick up a prescription, you might see two options on the receipt: the name you recognize from TV ads, or a simpler, cheaper version with a strange chemical name. You might wonder - is the cheaper one just as good? Or are you risking your health to save a few bucks?
The truth is simpler than the fear suggests. Generic drugs are not cheaper because they’re weaker. They’re cheaper because they don’t need to pay for advertising, fancy packaging, or years of research. The active ingredient - the part that actually treats your condition - is exactly the same as in the brand-name version. And the science backing this isn’t opinion. It’s hard data from thousands of studies and millions of patients.
How the FDA Makes Sure Generics Work the Same Way
The U.S. Food and Drug Administration (FDA) doesn’t just accept a generic drug because the company says it’s the same. They require proof - real, measurable proof - that it performs like the brand-name drug in your body. That proof comes from something called bioequivalence testing.
Here’s how it works: A small group of healthy volunteers takes both the brand-name drug and the generic version, in random order, with a break in between. Scientists then measure how much of the drug enters the bloodstream and how fast. Two key numbers matter: the peak concentration (Cmax) and the total exposure over time (AUC). For the generic to be approved, these numbers must fall within 80% to 125% of the brand-name drug’s values. That’s not a wide range - it’s tight. Most studies show differences of less than 4% in AUC and under 5% in Cmax.
Let’s put that in perspective. If a brand-name pill delivers 100 units of medicine into your blood, a generic could deliver anywhere from 80 to 125 units. But here’s the big myth busted: that doesn’t mean the generic contains only 80% of the active ingredient. It means the way your body absorbs it varies slightly - and even that variation is rare. In fact, 98% of bioequivalence studies show AUC differences under 10%.
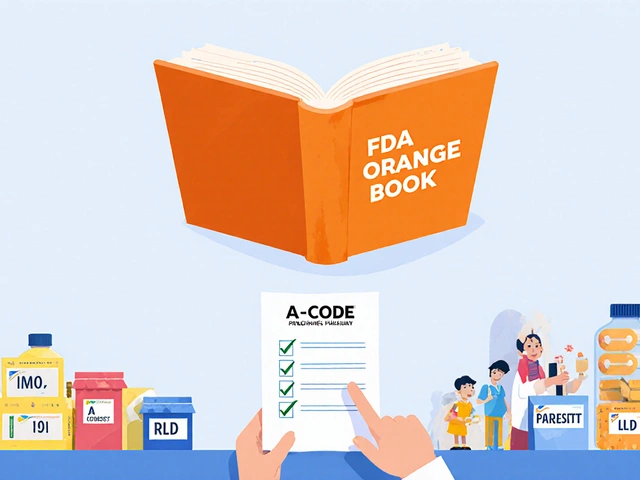
The FDA rates generics using a system. Most are labeled AB-rated, meaning they’re considered interchangeable with the brand. Some, like certain extended-release versions or complex formulations, get a B rating - meaning they’re approved but not automatically substituted. Your pharmacist will know which is which.
Real-World Results: Do Generics Actually Work?
Lab tests are one thing. Real patients are another. Did switching to a generic cause more heart attacks? More seizures? More hospital stays?
A 2020 study in Scientific Reports tracked over 1.2 million patients across 17 drug classes - including blood thinners, statins, and high blood pressure meds. After adjusting for age, health status, and other factors, researchers found that patients on generic versions had equal or better outcomes. In 10 out of 17 drugs, generics were linked to fewer deaths. In 11, they led to fewer major heart or brain events.
Another analysis of 38 cardiovascular trials found clinical equivalence in 35 of them - including all statins, beta-blockers, and ACE inhibitors. That’s not close. That’s conclusive.
Even drugs with a reputation for being tricky - like warfarin, used to prevent strokes - show no difference in outcomes when switched to a generic, as long as blood levels are monitored. A 2022 study in the American Journal of Managed Care found that while 61% of patients on warfarin asked for the brand name, their actual outcomes didn’t change when they took the generic.
Why People Still Don’t Trust Generics
If the science is so clear, why do so many people still hesitate?
One reason is marketing. Brand-name companies spend billions on ads that make their drugs feel like premium products. Generic drugs? They don’t run TV commercials. They’re invisible. That makes people assume they’re inferior - even when they’re not.
Another reason is inactive ingredients. Generics can use different fillers, dyes, or coatings. For most people, this makes zero difference. But for a small group - like those with severe allergies or rare digestive conditions - these extras can cause issues. That’s why some patients report feeling “off” after switching. It’s rarely the active drug. It’s the extra stuff.
A 2022 survey by Pharmacy Times found that 43% of patients believed generics were less effective. One in four refused substitution outright. Meanwhile, a GoodRx survey of over 8,000 users showed 89% reported no difference in how the drug worked - and most said cost was the biggest reason they switched.
Some conditions trigger more fear. Levothyroxine, used for hypothyroidism, is one. It’s a narrow therapeutic index (NTI) drug - meaning tiny changes in blood levels can matter. Even though studies show generic versions are safe and effective, many doctors and patients stick with the brand out of habit. The FDA and American Thyroid Association both say generics are fine, but they recommend checking thyroid levels 6-8 weeks after switching.

How Much Money Are You Saving?
Let’s talk numbers. In 2023, the average brand-name drug cost 80-85% more than its generic equivalent. That’s not a little. That’s life-changing.
Take Lipitor (atorvastatin), a cholesterol-lowering drug. The brand-name version cost $335 for a 30-day supply. The generic? $0.00 with a GoodRx coupon. Same pill. Same effect. Same safety profile.
Plavix (clopidogrel), used after heart attacks, was $450 for the brand. Generic? Again, $0.00 with a coupon.
Across the U.S. healthcare system, generics saved $373 billion in 2023. That’s not a guess. That’s from the Generic Pharmaceutical Association. It’s enough to cover health care for millions of uninsured people.
And it’s not just the U.S. Canada, the UK, and Germany have similar savings. Generics make medicine affordable. Without them, many people would skip doses - or skip treatment entirely.
When You Should Be Careful
Most of the time, switching to a generic is safe and smart. But there are exceptions.
NTI drugs - those with a narrow therapeutic index - need extra attention. Small changes in blood levels can cause big problems. These include:
- Warfarin (blood thinner)
- Levothyroxine (thyroid hormone)
- Phenytoin (seizure control)
- Lithium (mood stabilizer)
- Digoxin (heart failure)
For these, your doctor or pharmacist may recommend monitoring blood levels within 7-14 days after switching. That’s not because generics are unsafe. It’s because your body’s response matters more here. Think of it like tuning a guitar - even a small change in string tension can throw off the sound.
Also, some complex generics - like inhalers, topical creams, or injectables - require more testing to prove equivalence. The FDA approved 247 of these complex generics in 2023, up 19% from the year before. That’s progress. But it’s still an area where extra caution is wise.
What You Can Do
Here’s how to make the smart choice:
- Ask your pharmacist: “Is this generic AB-rated?” If yes, it’s interchangeable.
- Check the FDA’s Orange Book online - it lists all approved generics and their ratings.
- For NTI drugs, ask your doctor if a blood test is needed after switching.
- If you feel different after switching - fatigue, dizziness, mood changes - don’t assume it’s the drug. Talk to your provider. It could be an inactive ingredient, stress, or something else.
- Use tools like GoodRx or SingleCare to compare prices. Generics often cost pennies - even without insurance.
And if your doctor says, “I only prescribe the brand,” ask why. Is it because of evidence? Or habit? Most doctors are unaware that 78% of them correctly identify warfarin as needing monitoring - but only 32% know levothyroxine is an NTI drug. Knowledge gaps exist. You can help close them.
The Bigger Picture
Generics aren’t just about saving money. They’re about access. Without them, millions of people would be priced out of life-saving treatment. In 2023, 90% of all prescriptions filled in the U.S. were generics. That’s not a trend. That’s the new normal.
And the future? It’s getting better. New manufacturing tech, like AI-driven quality control, is making generics even more precise. A 2023 MIT study showed next-gen methods could reduce bioequivalence variation in warfarin generics to under 2% - almost identical to the brand.
Supply chain issues still cause shortages, especially with sterile injectables. But that’s a logistics problem, not a quality one. The science behind generics hasn’t changed. It’s stronger than ever.
So next time you see a generic on your prescription, don’t second-guess it. You’re not getting second-best. You’re getting the same medicine - at a fraction of the cost. And that’s not just smart. It’s powerful.







Shivam Goel November 25, 2025
Let’s be real-bioequivalence thresholds of 80-125%? That’s not precision; it’s a legal loophole dressed up as science. I’ve seen generics that made me dizzy, others that didn’t work at all. And yeah, the FDA says ‘98% are fine’-but what about the 2%? Who pays when your kidney fails because the filler changed? They don’t track adverse events in generics like they do for brands. And don’t get me started on the ‘same active ingredient’ myth-bioavailability isn’t just about the molecule; it’s about how your body handles it, and that’s personal.
Amy Hutchinson November 26, 2025
OMG YES. I switched my statin to generic and felt like a zombie for two weeks. My doctor laughed and said ‘it’s all in your head.’ Spoiler: it wasn’t. Turns out the generic had a dye I’m allergic to. No one told me. So yeah, science is cool-but your pharmacist should be REQUIRED to tell you if the filler changed. This isn’t cereal, it’s your bloodstream.
Archana Jha November 27, 2025
THEY’RE LYING TO YOU. The FDA? Owned by big pharma. The ‘bioequivalence’ tests? Done by the SAME companies making the generics. They pick the healthiest volunteers, give them the brand first, then the generic after a ‘break’-but what if your gut is messed up from stress? Or you’re on another med? They ignore that. And the 80-125% range? That’s a 45% swing. If your insulin was off that much, you’d be in the ER. They just don’t want you to know how much they’re gambling with your life for $0.50 a pill.
Aki Jones November 27, 2025
It’s not about the active ingredient. It’s about the excipients. And the FDA’s ‘AB-rated’ designation? A meaningless checkbox. The 2020 Scientific Reports study? Funded by the Generic Pharmaceutical Association. Conflict of interest? Please. And don’t even get me started on the fact that 43% of patients report ‘no difference’-but 72% of those same people had no baseline biomarkers before switching. Correlation ≠ causation. Also: levothyroxine? The FDA’s own data shows 18% of patients have TSH fluctuations after switching. That’s not ‘fine.’ That’s negligence.
Andrew McAfee November 28, 2025
Back home in Nigeria we don’t even have generics. We get the real stuff or nothing. People here think generics are some kind of miracle. But in places where you don’t have clean water or refrigeration for meds, the idea that ‘it’s the same’ is a luxury. I’ve seen people die because they couldn’t afford the brand. So yeah, save money. But don’t pretend it’s just about science. It’s about power. Who gets to live? Who gets to be a statistic?
Andrew Camacho November 29, 2025
Okay so let me get this straight-you’re telling me I should trust a pill that costs $0.01 because some lab in China says ‘it’s close enough’? Bro. I’ve had seizures. I’ve had heart palpitations. I’ve had doctors tell me ‘it’s just the generic.’ Guess what? I’m not a lab rat. I’m not your data point. And if you think I’m going to risk my life because some CEO wants to hit his quarterly earnings target, you’re delusional. I’ll pay $300 for Lipitor. I’ll pay $500. I’ll pay $1000. My life is not a cost-benefit analysis.
Patricia McElhinney November 30, 2025
While I appreciate the empirical rigor presented in the original post, I must respectfully contest the assertion that ‘generics are interchangeable.’ The pharmacokinetic variance, even within the 80–125% range, introduces non-trivial clinical risk for patients with comorbidities, polypharmacy, or compromised hepatic metabolism. Furthermore, the absence of longitudinal, real-world pharmacovigilance data for generic substitution in high-risk populations renders the ‘equal outcomes’ conclusion statistically premature. I would urge greater caution in public messaging.
Dolapo Eniola November 30, 2025
USA think they know everything. In Nigeria we use generics because we have no choice. And guess what? We don’t die. We don’t cry. We take it. Your fear is a luxury. Your brand names? Made in China. Your ‘FDA-approved’? Same factory as the generic. You think you’re safe? You’re just paying for a logo. And you call us poor? We’re the ones who survived. You’re the ones who got brainwashed by ads. 💪
Agastya Shukla December 1, 2025
Interesting breakdown. One thing I’d add: the 2023 MIT study on AI-driven quality control for warfarin generics is actually a game-changer. If we can reduce variability to under 2%, we’re approaching pharmaceutical-grade consistency without the brand markup. That’s not just cost savings-it’s equity. But the real issue isn’t science. It’s trust. And trust isn’t built with data. It’s built with transparency. If pharmacies started labeling generic batches with lot numbers and manufacturing origins, like food labels, people would feel safer. Not because the drug changes-but because they feel seen.