Understanding Menopause and Urinary Incontinence
As a woman, I know that menopause is a natural part of the aging process. However, it can bring about some uncomfortable and sometimes embarrassing symptoms, one of which is urinary incontinence. It's essential to understand the connection between menopause and urinary incontinence to find solutions that can help alleviate this issue.
In this article, I'll discuss the causes of urinary incontinence during menopause and offer some practical solutions to help manage this condition. So, let's dive in and explore the world of menopause and urinary incontinence!
The Role of Hormones in Menopause and Urinary Incontinence
During menopause, our bodies undergo a significant hormonal shift. Estrogen, a hormone that plays a crucial role in maintaining the strength and elasticity of our pelvic muscles and tissues, declines. This decline in estrogen levels can lead to the weakening of the pelvic floor muscles, making it more difficult for us to control our bladder and, as a result, causing urinary incontinence.
Moreover, the decrease in estrogen levels can also cause the lining of the urethra to thin, leading to a weaker urinary sphincter. This weakening can make it harder to hold urine in and can contribute to incontinence issues.
Types of Urinary Incontinence During Menopause
There are different types of urinary incontinence that we may experience during menopause, and understanding them can help us find the right solutions. The two most common types are stress incontinence and urge incontinence.
Stress Incontinence
Stress incontinence occurs when pressure is placed on the bladder, causing involuntary leakage. This pressure can be caused by activities such as laughing, sneezing, coughing, or exercising. The weakening of the pelvic floor muscles and the thinning of the urethra lining due to declining estrogen levels can contribute to stress incontinence during menopause.
Urge Incontinence
Urge incontinence, also known as overactive bladder, is characterized by a sudden and intense need to urinate, often followed by involuntary leakage. This type of incontinence can be caused by several factors during menopause, including hormonal changes and a decline in bladder capacity.
Practical Solutions to Manage Menopause-Related Urinary Incontinence
Now that we have a better understanding of the causes of urinary incontinence during menopause, let's discuss some practical solutions that can help us manage this condition.
Pelvic Floor Muscle Exercises
One of the most effective ways to strengthen our pelvic floor muscles and improve bladder control is by performing pelvic floor muscle exercises, also known as Kegel exercises. These exercises involve contracting and relaxing the muscles that control the flow of urine. By practicing Kegel exercises regularly, we can strengthen our pelvic floor muscles and reduce urinary incontinence.
Bladder Training
Bladder training is another useful technique for managing urinary incontinence during menopause. This method involves gradually increasing the time between urination, helping to train our bladder to hold more urine for more extended periods. Bladder training can help improve both stress and urge incontinence.
Lifestyle Changes
Making some lifestyle changes can also help us manage urinary incontinence during menopause. Reducing our intake of caffeine, alcohol, and spicy foods can help decrease bladder irritation, while maintaining a healthy weight can help reduce pressure on the pelvic floor muscles. Additionally, quitting smoking can improve our overall bladder health.
Hormone Replacement Therapy (HRT)
For some women, hormone replacement therapy (HRT) can help alleviate urinary incontinence during menopause. HRT involves taking estrogen to help balance hormone levels and improve the strength of the pelvic floor muscles. However, it's essential to discuss the potential risks and benefits of HRT with a healthcare professional before deciding on this treatment option.
Medical Treatments for Menopause-Related Urinary Incontinence
If lifestyle changes and non-invasive treatments aren't enough to manage urinary incontinence during menopause, there are medical treatment options available that can help.
Medications
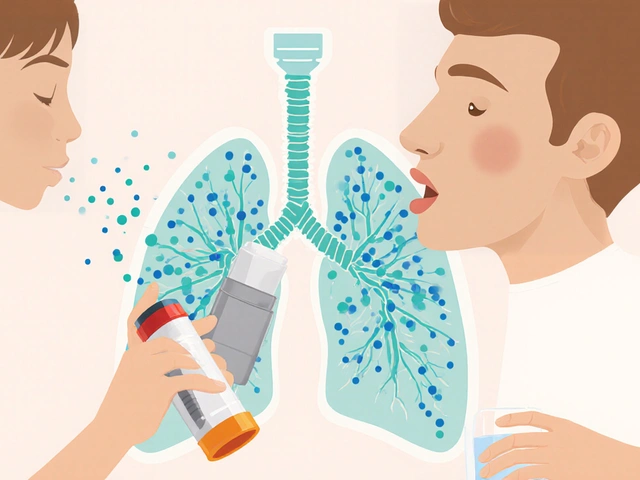
There are medications available that can help relax the bladder muscles and prevent involuntary contractions, which can help manage urge incontinence. A healthcare professional can discuss the various medication options and help determine the best course of treatment for our individual needs.
Surgical Options
In some cases, surgical intervention may be necessary to treat urinary incontinence during menopause. Surgical options can include procedures such as a sling procedure or a bladder neck suspension, which help support the urethra and bladder neck. It's essential to discuss these surgical options and their potential risks and benefits with a healthcare professional.
Conclusion
Urinary incontinence during menopause can be an uncomfortable and sometimes embarrassing issue, but it's essential to remember that it's a common condition and that there are solutions available to help manage it. By understanding the causes of menopause-related urinary incontinence and exploring various treatment options, we can find the best solution to improve our overall quality of life during this stage of our lives.






Sunil Rawat May 15, 2023
Hey folks! Menopause can be a tricky time, especially when the bladder decides to act up.
It's really just the drop in estrogen that makes the pelvic floor a bit lazy.
Doing Kegels daily can give those muscles a nice shout‑out.
Also, sipping water instead of coffee can keep the bladder calm.
Stay strong!
Andrew Buchanan May 15, 2023
The hormonal shift does affect urinary control.
Krishna Chaitanya May 15, 2023
Wow wow wow the stress incontinence hits like a surprise party that nobody wanted it hits hard the urge is like fireworks in the night
diana tutaan May 15, 2023
Honestly the article glosses over the fact that many women simply can't tolerate hormone therapy it's a risky gamble that the piece fails to emphasize
Sarah Posh May 15, 2023
Remember, you are not alone and every small step, like a short walk or a mindful breathing session, can boost confidence in managing symptoms.
James Knight May 15, 2023
Yeah right, just do Kegels and quit coffee? As if it's that easy, the stress you feel is real and this fluff doesn't cut it.
Ajay D.j May 15, 2023
Friends, think of your body as a temple; a few minutes of pelvic floor training each day can bring balance and peace, trust the process.
Dion Campbell May 15, 2023
One must question whether the author truly grasped the complexities of uro‑gynecological dynamics, for the discourse remains superficial at best.
Burl Henderson May 15, 2023
From a urodynamic perspective, enhancing sphincteric competency via biofeedback‑modulated pelvic floor training can synergistically reduce detrusor overactivity.
Leigh Ann Jones May 15, 2023
While the piece offers a decent overview of the hormonal mechanisms behind menopause‑related urinary leakage, it stops far short of delivering actionable depth.
The recommendation to simply 'try Kegels' is presented without any reference to proper technique, frequency, or the importance of progressive overload.
Moreover, the omission of pelvic floor physiotherapy as a viable clinical option feels like an oversight that could mislead readers.
Patients often benefit from electromyographic feedback, yet this nuance is entirely absent.
The lifestyle advice, though well‑meaning, lists caffeine and alcohol reduction without acknowledging individual tolerance variability.
A one‑size‑fits‑all disclaimer does little to empower women navigating complex comorbidities.
In addition, the discussion of hormone replacement therapy fails to address the latest data on selective estrogen receptor modulators, which could be a game‑changer for some.
The surgical section glosses over potential complications such as mesh erosion, infection, and postoperative voiding dysfunction.
Readers deserve a balanced risk‑benefit analysis rather than a cursory list of procedures.
On the positive side, the article correctly highlights bladder training as a cornerstone of behavioral therapy.
Nevertheless, the lack of structured protocols-like the timed voiding schedule-leaves the advice feeling incomplete.
It would have been helpful to include patient‑reported outcome measures like the ICIQ‑SF to gauge treatment efficacy.
A brief mention of emerging therapies, such as laser vaginal rejuvenation, would have demonstrated awareness of evolving standards.
Instead, the narrative remains anchored in traditional approaches, ignoring the nuanced spectrum of patient preferences.
In short, the article serves as a superficial primer rather than a comprehensive guide for clinicians or patients seeking depth.
Future revisions should integrate evidence‑based details, multidisciplinary perspectives, and realistic expectations to truly support those affected.