Antidepressant Choice Calculator
Asendin (amoxapine) isn’t one of the first names you hear when people talk about antidepressants. But for some people, it’s the one that finally worked after trying everything else. It’s a tricyclic antidepressant (TCA), older than Prozac but still used - especially when newer drugs fail. If you’ve been on SSRIs like sertraline or fluoxetine without relief, or if you’re dealing with depression mixed with anxiety or even mild psychotic symptoms, amoxapine might be on your doctor’s radar. But it’s not for everyone. This isn’t a simple switch. It comes with side effects, risks, and a lot of variables. So how does it stack up against other options? Let’s break it down.
What Is Amoxapine (Asendin) Really?
Amoxapine is a tricyclic antidepressant approved by the FDA in the 1980s. It’s not just another TCA. Unlike older ones like amitriptyline or nortriptyline, amoxapine has a unique chemical twist: it breaks down into a compound called 7-hydroxyamoxapine, which acts like a weak antipsychotic. That’s why it’s sometimes prescribed for depression with anxiety, agitation, or even mild hallucinations - situations where SSRIs often fall short.
It works by blocking the reuptake of serotonin and norepinephrine, similar to other TCAs. But its dopamine-blocking effect gives it an edge in cases where mood is stuck, and thoughts are racing or distorted. It’s not a first-line treatment, though. Doctors usually try SSRIs or SNRIs first because they’re safer and easier to tolerate.
Typical doses range from 50 mg to 300 mg per day, split into two doses. It takes 2 to 6 weeks to kick in - same as most antidepressants. But unlike some newer drugs, amoxapine doesn’t come in extended-release form, so you’ll need to take it twice a day.
Common Side Effects of Amoxapine
Every antidepressant has side effects. But amoxapine’s list is longer and more intense than most modern options.
- Drowsiness - very common, especially at first. Many people can’t drive or operate machinery for the first few weeks.
- Dry mouth - so bad that some people chew sugar-free gum constantly.
- Constipation - often worse than with SSRIs.
- Blurred vision - temporary but annoying.
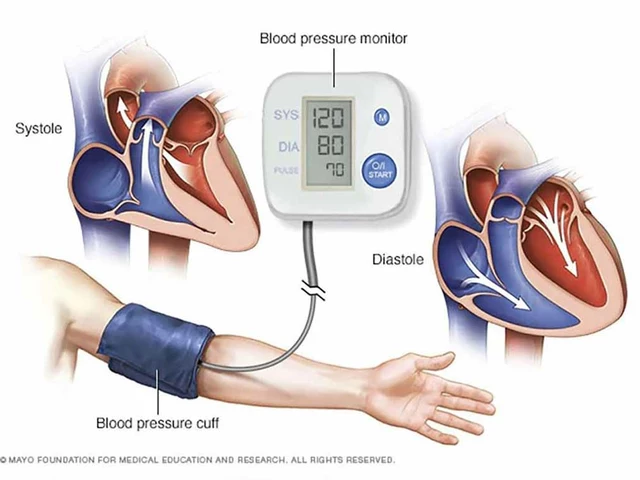
- Dizziness or low blood pressure - especially when standing up fast. This can lead to falls in older adults.
- Weight gain - not as bad as with amitriptyline, but still noticeable for some.
- Seizure risk - higher than with SSRIs. People with a history of seizures are usually kept off it.
- Cardiac issues - it can prolong the QT interval on an ECG, which increases risk of dangerous heart rhythms. This is why doctors check heart health before starting it.
There’s also a rare but serious risk: neuroleptic malignant syndrome (NMS), a life-threatening reaction to dopamine-blocking drugs. Symptoms include high fever, stiff muscles, confusion, and sweating. If this happens, you need emergency care.
Amoxapine vs. SSRIs: Sertraline, Fluoxetine, Escitalopram
SSRIs are the go-to for depression today. They’re safer, have fewer side effects, and are easier to stop. But they don’t work for everyone. About 30% of people don’t respond to the first SSRI they try.
Here’s how amoxapine compares:
| Feature | Amoxapine (Asendin) | SSRIs (e.g., Sertraline, Fluoxetine) |
|---|---|---|
| Effectiveness for depression | Similar to SSRIs, but better for depression with anxiety or agitation | Good for mild to moderate depression; less effective for severe or psychotic features |
| Onset of action | 2-6 weeks | 2-6 weeks |
| Common side effects | Drowsiness, dry mouth, constipation, dizziness, weight gain, cardiac risks | Nausea, sexual dysfunction, insomnia, weight gain (mild), headache |
| Overdose risk | High - can be fatal | Low - rarely fatal in overdose |
| Drug interactions | Many - especially with other CNS depressants, antihypertensives, and heart meds | Moderate - mainly with MAOIs and blood thinners |
| Use in elderly | Not preferred - higher fall and heart risk | Preferred first choice |
SSRIs win on safety. If you’re young, healthy, and have mild depression, they’re the clear first choice. But if you’ve tried two or three SSRIs and still feel stuck - especially if you’re irritable, restless, or have racing thoughts - amoxapine might be the next step.
Amoxapine vs. SNRIs: Venlafaxine, Duloxetine
SNRIs like venlafaxine (Effexor) and duloxetine (Cymbalta) work on both serotonin and norepinephrine, just like amoxapine. But they don’t block dopamine. That’s the big difference.
SNRIs are often used for depression with chronic pain - duloxetine is FDA-approved for fibromyalgia and diabetic nerve pain. Venlafaxine is effective for severe depression and sometimes used when SSRIs fail.
Compared to amoxapine:
- SNRIs have fewer anticholinergic side effects (dry mouth, constipation, blurred vision).
- They’re safer in overdose.
- But they can cause high blood pressure at higher doses (especially venlafaxine).
- They don’t help with agitation or psychotic symptoms the way amoxapine sometimes does.
For someone with depression and severe anxiety or agitation, amoxapine may offer more relief. For someone with depression and back pain, duloxetine might be better. It’s about matching the drug to the symptom profile.
Amoxapine vs. Other TCAs: Amitriptyline, Nortriptyline
Amoxapine is one of the newer TCAs. Older ones like amitriptyline and nortriptyline are more commonly used, especially in Australia and Europe.
Amitriptyline is strong for pain and sleep, but it’s also the most sedating and has the worst side effect profile. Nortriptyline is a metabolite of amitriptyline - it’s cleaner, with fewer anticholinergic effects.
Here’s the key: amoxapine’s antipsychotic edge makes it unique among TCAs. If you’re dealing with depression that feels "foggy" or "paranoid," amoxapine might help where others don’t. But if you just need better sleep and less pain, nortriptyline might be a safer bet.
Both amitriptyline and nortriptyline are cheaper than amoxapine - especially in Australia, where generics are widely available. Amoxapine is still under brand name in many places, so cost can be a barrier.
When Is Amoxapine a Good Choice?
It’s not a first-line drug. But here are scenarios where it makes sense:
- You’ve tried at least two SSRIs and one SNRI with no improvement.
- Your depression includes severe anxiety, agitation, or irritability.
- You have mild psychotic features - like believing people are talking about you, or hearing whispers.
- You’re not elderly and don’t have heart problems.
- You’re willing to tolerate side effects for a chance at better results.
It’s also sometimes used off-label for treatment-resistant depression, especially in private psychiatric practices. But it’s not something you should ask for on your own. Your doctor needs to monitor you closely - especially for heart rhythm changes and blood pressure.
When Should You Avoid Amoxapine?
Don’t take amoxapine if you:
- Have a history of heart attack, arrhythmias, or QT prolongation.
- Have seizures or epilepsy.
- Are under 18 - it’s not approved for children.
- Are taking MAO inhibitors (like phenelzine) - you must wait at least 14 days after stopping an MAOI before starting amoxapine.
- Are pregnant or breastfeeding - data is limited, and risks are unclear.
- Are over 65 - increased risk of falls, confusion, and heart issues.
Also, never mix it with alcohol, benzodiazepines, or sleep aids. The combination can slow your breathing to dangerous levels.
Alternatives If Amoxapine Doesn’t Work or Isn’t Right
If amoxapine isn’t working, or the side effects are too much, here are other options:
- Mirtazapine (Remeron) - helps with sleep and appetite, less sexual side effects. Good for people who’ve lost weight or can’t sleep.
- Bupropion (Wellbutrin) - doesn’t cause sexual side effects or weight gain. Good for low energy and lack of motivation.
- Vortioxetine (Trintellix) - newer, targets multiple serotonin receptors. Helps with brain fog and memory issues.
- Psychotherapy + medication - CBT or interpersonal therapy paired with any antidepressant often works better than meds alone.
- ESCT or TMS - if you’ve tried four or more meds with no success, electroconvulsive therapy (ECT) or transcranial magnetic stimulation (TMS) may be next steps.
There’s no magic pill. But there are options. The key is working with a doctor who understands your full picture - not just the depression, but your sleep, energy, anxiety, pain, and life stress.
Final Thoughts: Is Amoxapine Worth It?
Amoxapine isn’t a miracle drug. It’s a tool - a blunt one, with heavy risks. But for some people, it’s the only thing that lifted the fog. If you’ve been stuck for months, or even years, and every other antidepressant left you feeling half-alive, it might be worth a careful trial.
But don’t rush it. Get your heart checked. Tell your doctor everything - even the weird thoughts you’re afraid to say out loud. And give it time. Don’t quit after two weeks because you still feel tired. It takes weeks to work. And if it does work, don’t stop suddenly. Withdrawal can cause dizziness, nausea, and even rebound anxiety.
There’s no shame in trying something different. Depression is complicated. The right drug isn’t always the newest one. Sometimes, it’s the one that’s been around for 40 years - if it fits you.
Is Asendin (amoxapine) still used today?
Yes, but rarely as a first choice. It’s mostly used today for treatment-resistant depression, especially when there’s significant anxiety, agitation, or mild psychotic symptoms. It’s not common in Australia or the U.S. because newer drugs are safer, but it’s still prescribed by psychiatrists when other options fail.
Can I switch from an SSRI to amoxapine?
You can, but you must stop the SSRI first and wait at least one to two weeks before starting amoxapine. This prevents serotonin syndrome - a dangerous buildup of serotonin. Always do this under a doctor’s supervision.
Does amoxapine cause weight gain?
Yes, it can. While not as severe as amitriptyline, many people gain 5-10 pounds over a few months. If weight is a concern, your doctor might consider bupropion or vortioxetine instead.
Is amoxapine better than lithium for depression?
They’re used for different things. Lithium is mainly for bipolar disorder, not unipolar depression. Amoxapine is for major depression. Sometimes, lithium is added to an antidepressant like amoxapine to boost its effect - but they’re not direct alternatives.
How long does it take for amoxapine to work?
Most people start noticing small improvements in mood and energy after 2-3 weeks. Full effects usually take 4-6 weeks. Don’t give up before then, even if side effects are tough at first.
Can amoxapine cause suicidal thoughts?
Like all antidepressants, amoxapine carries a black box warning for increased risk of suicidal thoughts in people under 25. This risk is highest in the first few weeks of treatment or after a dose change. If you or someone you know feels worse or has new thoughts of self-harm, contact a doctor immediately.
Is amoxapine addictive?
No, amoxapine is not addictive. You won’t get high from it, and it doesn’t cause cravings. But stopping it suddenly can cause withdrawal symptoms like dizziness, nausea, and anxiety. Always taper off slowly with medical guidance.
If you’re considering amoxapine, talk to a psychiatrist - not just your GP. They’ll check your heart, review your full history, and help you weigh the risks against the potential benefits. Depression is hard. But you don’t have to keep trying the same thing over and over. There are other paths - and sometimes, the old ones still work.






Clyde Verdin Jr October 30, 2025
This post is literally a 10-page essay disguised as a Reddit thread. 🤡 I’ve been on amoxapine for 8 months and it turned my brain from a broken toaster to a Tesla. SSRIs made me feel like a zombie who forgot how to laugh. Amoxapine? I cried during a commercial for dog food. For the first time in 5 years. 🥲
Jay Wallace November 1, 2025
Okay but… have you even READ the FDA label? Amoxapine? That’s a 1980s relic. You think you’re some kind of rebel for taking it? In Europe they use… well… ACTUAL medicine. Not… this… dinosaur. And don’t even get me started on the QT prolongation. You’re playing Russian roulette with your heart. And you call that treatment??
Alyssa Fisher November 2, 2025
I think what’s really interesting here is how we’ve normalized the idea that depression is a problem to be solved with chemistry alone. Amoxapine’s dopamine-blocking effect isn’t just pharmacological-it’s almost philosophical. It doesn’t just lift mood, it quiets the noise. But we don’t talk about the cost of that silence. What happens when the fog lifts, and you’re left with the raw, unfiltered truth of your life? That’s the real treatment.
Alyssa Salazar November 3, 2025
Okay so let’s get real-amoxapine’s antipsychotic metabolite? That’s the MVP. SSRIs don’t touch the agitation, the rumination, the paranoid whispers. I had a patient who thought her cat was transmitting government messages. Sertraline? Nope. Amoxapine? 3 weeks in, she was feeding the cat and watching Netflix. That’s not a side effect. That’s a damn miracle. Stop acting like it’s some dangerous outlier-it’s a precision tool.
Beth Banham November 4, 2025
I’ve been on three different meds over six years. None worked. I didn’t even dare ask about amoxapine. I was scared. But reading this made me feel… seen. Not judged. Just… understood. I’ll talk to my psychiatrist next week. Thanks for writing this.
Brierly Davis November 5, 2025
You’re not alone. I was on fluoxetine for 18 months. Felt like a ghost. Then my doc switched me to amoxapine. First two weeks? I slept 14 hours a day. Felt like I was drowning in syrup. But week 5? I cooked my first real meal in two years. I cried. Not sad tears. Happy ones. You’re doing the right thing by researching. 💪
Amber O'Sullivan November 7, 2025
I’ve been on amoxapine since 2021 and I’m still here breathing so it works for me. I dont care what the manual says. My heart is fine. My mind is clear. The dry mouth sucks but I drink water. End of story
Jim Oliver November 8, 2025
Wow. Just… wow. You wrote a 2,000-word love letter to a drug that can kill you if you sneeze wrong. And you call this ‘helpful’? This isn’t medicine-it’s Russian roulette with a prescription pad. If you’re not in a psychiatric ward, you shouldn’t be near this stuff. And yes, I’m a doctor. And yes, I’ve seen the aftermath.
William Priest November 8, 2025
Amoxapine? LOL. I’m a neuropharm grad. You think you’re edgy taking a TCA? Try real science: ketamine infusions, psilocybin trials, or even deep TMS. Amoxapine is like using a horse and buggy when you’ve got a Tesla. And the side effects? Bro, you’re gonna have a heart attack at 45 because you listened to some guy on Reddit. 🤦♂️
Jennifer Bedrosian November 9, 2025
I took this for 3 months and I swear I turned into a zombie who forgot how to smile. Dry mouth so bad I chewed gum till my jaw locked. And the dizziness? I fell down my stairs. Bro. Just… no. I’d rather be sad than feel like my body’s betraying me every second. I’m back on sertraline and I’m okay with it. Sad but alive
Lashonda Rene November 9, 2025
I just want to say I’ve been depressed for 12 years and I’ve tried like 10 different meds and I thought I was broken but reading this made me feel like maybe there’s still hope. I didn’t even know amoxapine existed until now. I’m gonna tell my doctor about it. I know it sounds scary but I’m tired of feeling like a shadow. I’m tired of being tired. Maybe this is the one. I don’t know. But I’m gonna try. I just needed to say that out loud.
Andy Slack November 9, 2025
I’ve been on amoxapine for 11 months. I don’t talk about it much. People think I’m crazy. But I can finally focus. I finished my degree. I got a job. I went on a date. I didn’t cry for three weeks straight. It’s not perfect. I still get dry mouth. I still have to take it twice a day. But it gave me back my life. I’m not grateful. I’m just… here.
Rashmi Mohapatra November 10, 2025
This is why India has better mental health care. We don’t waste time on these old toxic drugs. We use yoga, meditation, ayurveda, and community. Amoxapine? Sounds like Western pharmaceutical greed. You think chemicals fix trauma? Nah. Your pain needs love, not pills.
Steve Phillips November 10, 2025
Let me just say-this entire post is a glorified drug commercial. You’re acting like amoxapine is some secret weapon. It’s not. It’s a last-resort chemical sledgehammer. And you know what? The fact that you’re even considering it means your doctor is either desperate… or lazy. There are better options. You just refuse to look because you want the quick fix. Pathetic.
Key Davis November 10, 2025
As a psychiatrist with over 25 years of clinical experience, I can confirm that amoxapine remains a clinically valid, albeit underutilized, option in the treatment-resistant depression paradigm. Its unique pharmacological profile, particularly its metabolite-mediated dopaminergic antagonism, provides a distinct therapeutic niche. However, its use necessitates rigorous cardiac screening, baseline ECG, and ongoing QT interval monitoring. I routinely prescribe it in cases where serotonin-dominant agents have failed, particularly in patients with comorbid anxiety-agitation syndromes. The risk-benefit ratio, when properly managed, is favorable.
Brad Seymour November 12, 2025
I’m from the UK and we use amoxapine more than you think. Not often, but when it works? It’s like someone turned the volume down on the screaming in your head. I had a friend on it. She was catatonic on SSRIs. After two months on amoxapine? She started painting again. Didn’t fix everything. But it gave her back a piece of herself. That’s worth the dry mouth.
Malia Blom November 13, 2025
I read this and I thought-this is what happens when you give a pharmacology textbook a personality. Amoxapine isn’t a miracle. It’s a compromise. A trade-off. You trade sleep, safety, and stability for… maybe a sliver of clarity. And that’s okay. Sometimes the best medicine isn’t the safest one. It’s the one that lets you feel human again-even if it costs you your appetite, your balance, and your peace of mind.