Loperamide: What It Is, How It Works, and What You Need to Know
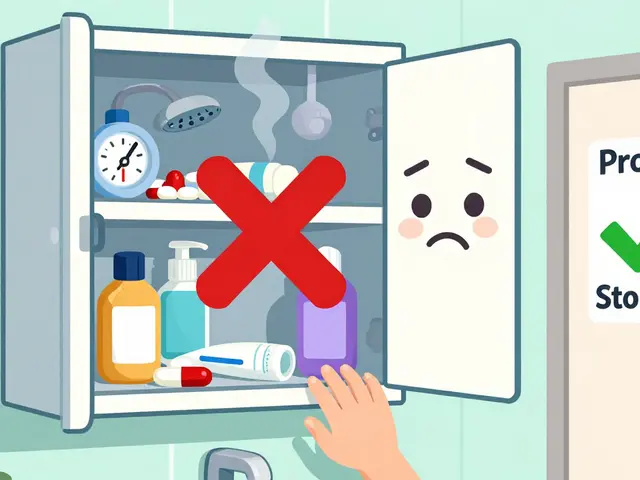
When you’re stuck with sudden diarrhea, loperamide, a widely used over-the-counter anti-diarrheal medication that slows gut movement by acting on opioid receptors in the intestines. Also known as Imodium, it’s one of the most common pills kept in medicine cabinets across the U.S. and Europe. But it’s not just a quick fix—it’s a drug with real risks if used wrong. Unlike painkillers like morphine, loperamide doesn’t cross the blood-brain barrier easily at normal doses, which is why it doesn’t cause euphoria or strong sedation. But take too much, and that barrier breaks down. There have been real cases of heart rhythm problems, even deaths, from people taking way more than the label says—sometimes to get high, sometimes because they thought more meant faster relief.
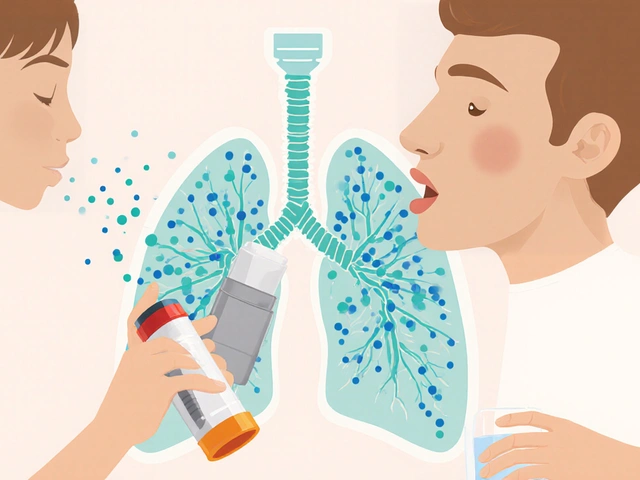
It’s a opioid receptor agonist, a type of drug that binds to opioid receptors in the body, primarily in the gut, but it’s not classified as a controlled substance in most places. That’s partly why people underestimate it. It’s sold next to pain relievers and antacids, but it’s not the same as ibuprofen. It works locally in the intestines to reduce contractions, letting stool move slower so water gets reabsorbed. That’s why it helps with acute diarrhea from food poisoning or stomach bugs. But if your diarrhea lasts more than two days, or if you have a fever, bloody stool, or are dehydrated, loperamide isn’t the answer—you need to see a doctor. And if you’re on other meds, like certain antibiotics or antidepressants, it can interact in ways you won’t expect. One study found that combining loperamide with drugs that slow its breakdown in the liver can spike blood levels dangerously, even at normal doses.
It’s also not for kids under two, and it shouldn’t be used for chronic conditions like IBS without a doctor’s direction. Many people don’t realize that diarrhea is often your body’s way of flushing out something harmful. Stopping it too soon might trap bacteria or toxins inside. And while it’s safe for short-term use, long-term reliance can mess with your gut’s natural rhythm. If you’ve ever taken it for a week straight because your stomach "just isn’t right," you’re not alone—but you’re also not safe.
What you’ll find below are real, practical posts about how loperamide fits into the bigger picture of medication safety, drug interactions, and when to avoid self-treatment. You’ll see how it compares to other anti-diarrheal options, why pharmacists warn against overuse, and how it ties into broader issues like opioid misuse and over-the-counter drug risks. These aren’t generic advice pieces—they’re grounded in the same kind of real-world cases and clinical data that pharmacists and doctors use every day. Whether you’re using it now, thinking about it, or just want to understand why your doctor asked if you’ve been taking it, this collection gives you what you need to make smart choices.
Diarrhea: Understanding Acute vs. Chronic and When Antimotility Drugs Help
Understand the difference between acute and chronic diarrhea, when to use antimotility drugs like loperamide, and what to do when diarrhea lasts more than two weeks. Get the facts on causes, risks, and real treatment options.