Lidocaine Overdose: Signs, Risks, and What to Do
When lidocaine, a common local anesthetic used in dental procedures, skin treatments, and nerve blocks. Also known as Xylocaine, it’s one of the most widely used numbing agents in medicine. But too much—whether from accidental injection, skin absorption, or mixing with other drugs—can turn a safe treatment into a medical emergency. Lidocaine overdose doesn’t always come with a warning. It can sneak up fast, especially if you’re using multiple products at once or have liver problems that slow how your body clears it.
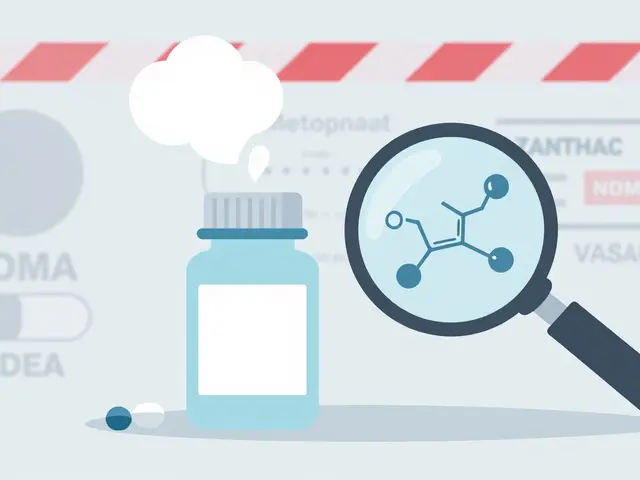
It’s not just about how much you take—it’s about how your body handles it. People with liver disease, older adults, or those on certain heart or antidepressant meds are at higher risk because their systems can’t break down lidocaine quickly. local anesthetic toxicity, the medical term for when lidocaine builds up to dangerous levels in the blood starts with tingling in the mouth, a metallic taste, or ringing in the ears. Then comes dizziness, blurred vision, muscle twitching, and confusion. If it gets worse, seizures, slow breathing, or even cardiac arrest can follow. The toxic levels of lidocaine, the concentration in blood that triggers serious side effects is around 5–12 mcg/mL, but some people react at lower levels. That’s why doctors check your weight, medical history, and how much you’ve already taken before giving a dose.
Many overdoses happen outside hospitals—using numbing creams or patches too often, applying them to large areas, or using them on broken skin. A single lidocaine patch is safe for most people, but putting on five at once? That’s asking for trouble. Same with over-the-counter sprays used for sore throats or mouth ulcers. People think, "It’s just a numbing agent," but that’s like saying, "It’s just a painkiller," and then taking ten pills. The lidocaine side effects, the body’s reaction to too much of the drug aren’t always obvious until it’s too late.
If you or someone else shows signs of overdose—slurred speech, trouble breathing, or a seizure—call emergency services right away. Don’t wait. Don’t try to "sleep it off." Lidocaine overdose needs fast medical care: oxygen, IV fluids, and sometimes medications to stop seizures or support heart function. There’s no antidote, but treatment works if it’s quick.
The posts below give you real, practical info on how lidocaine fits into the bigger picture of drug safety. You’ll find guides on spotting dangerous medication reactions, understanding black box warnings, reading FDA labels, and avoiding hidden risks with common treatments. Whether you’re a patient using lidocaine patches, a caregiver, or just someone trying to stay safe with over-the-counter meds, these articles help you connect the dots—before something goes wrong.
OTC Topical Pain Relievers: Creams, Gels, and Patches Safety Guide
Learn the real risks and safe usage tips for OTC topical pain relievers like creams, gels, and patches. Avoid burns, lidocaine overdose, and hidden dangers with expert-backed advice.