Relapse Risk: What It Means and How to Reduce It
When someone is recovering from addiction, chronic illness, or mental health struggles, relapse risk, the chance that symptoms return after improvement. Also known as recurrence risk, it’s not a sign of failure—it’s a biological reality shaped by brain chemistry, medication gaps, and lifestyle triggers. Many assume relapse happens because a person didn’t try hard enough. But studies show it’s often linked to how drugs interact with the body, how well treatment is maintained, and whether support systems are in place. For example, someone on opioids for pain might stop taking their meds too soon after surgery, triggering withdrawal—and with it, a strong urge to return to the drug. That’s not weakness. That’s opioid withdrawal, a physiological response to stopping long-term opioid use kicking in hard.
Relapse risk doesn’t just apply to addiction. It’s also critical in managing conditions like depression, bipolar disorder, or even heart disease. Stopping an antidepressant too fast? High relapse risk. Skipping blood pressure meds for a few days? Same thing. The medication adherence, how consistently a patient takes their prescribed drugs is one of the biggest factors. A 2021 study in the Journal of Clinical Psychiatry found that people who missed just two doses of their mood stabilizer in a month were three times more likely to have a manic or depressive episode. And it’s not just about forgetting pills. Side effects like drowsiness from antipsychotics or constipation from opioids can make people quit without telling their doctor. That’s why black box warnings, the FDA’s strongest alerts for life-threatening drug risks exist—to flag when stopping suddenly could be deadly.
Reducing relapse risk isn’t about willpower alone. It’s about smart systems: using pill organizers, scheduling check-ins with a provider, avoiding known triggers like stress or certain social settings, and understanding how your meds work. For example, if you’re on a fentanyl patch, quitting cold turkey can cause severe withdrawal—so tapering under medical supervision cuts relapse risk dramatically. Or if you’re using budesonide for asthma, skipping doses might seem harmless, but it can lead to a flare-up that feels like a relapse. Even something as simple as fiber supplements can interfere with absorption of meds like levothyroxine, quietly increasing the chance your treatment stops working. Relapse risk isn’t a mystery—it’s a chain of small, manageable decisions. The posts below break down exactly how these chains form, what breaks them, and how to build stronger ones.
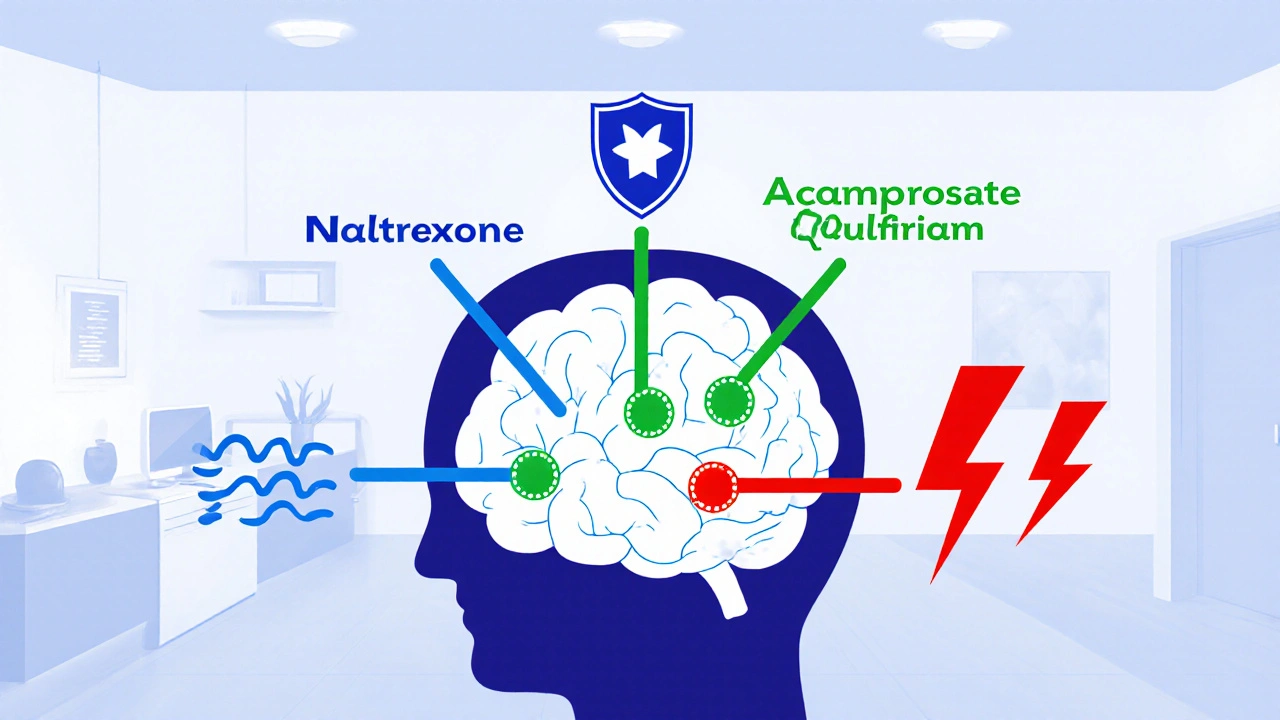
Medications for Alcohol Use Disorder: How They Reduce Relapse Risk - and When They Don’t
Naltrexone, acamprosate, and disulfiram can reduce relapse risk in Alcohol Use Disorder - but only if used correctly. Learn how they work, who they help, and why so few people get them.