Allergic Rhinitis: What You Need to Know
Did you know that nearly one in three adults deals with sneeze‑fits, runny nose, or itchy eyes every pollen season? When working with Allergic Rhinitis, a chronic inflammation of the nasal passages triggered by common allergens such as pollen, dust mites, or animal dander, you’re facing more than just a seasonal nuisance. It’s a condition that can mess with sleep, concentration, and even mood. Below we break down the big picture so you can see how the pieces fit together.
Triggers and Related Conditions
One of the main drivers of allergic rhinitis is Pollen Allergy, an immune response to tiny plant particles that float in the air during spring and summer. When pollen lands in the nose, the body releases histamine, causing the classic symptoms. But pollen isn’t the only culprit; indoor allergens like dust mites and pet dander act the same way. These triggers often overlap with Eye Allergies, inflammation of the conjunctiva that leads to red, itchy eyes, creating a full‑body reaction. Many people also notice a link between allergic rhinitis and sinus pressure, which can develop into sinusitis if left unchecked.
Understanding these connections helps you target the right solution. For example, if you notice symptoms flare up only when the grass is blooming, pollen is likely the primary trigger. If they persist indoors year‑round, dust mites might be the hidden factor. Recognizing the source lets you take smarter steps—like using air filters or swapping bedding for allergen‑proof covers.
How Treatment Choices Fit Together
The first line of defense often includes Antihistamines, medications that block histamine receptors to reduce sneezing, itching, and runny nose. They’re quick, over‑the‑counter, and work well for occasional flare‑ups. However, when symptoms are persistent, doctors may recommend Nasal Corticosteroids, sprays that reduce inflammation directly in the nasal lining for long‑term control. These sprays address the root inflammation rather than just the histamine reaction.
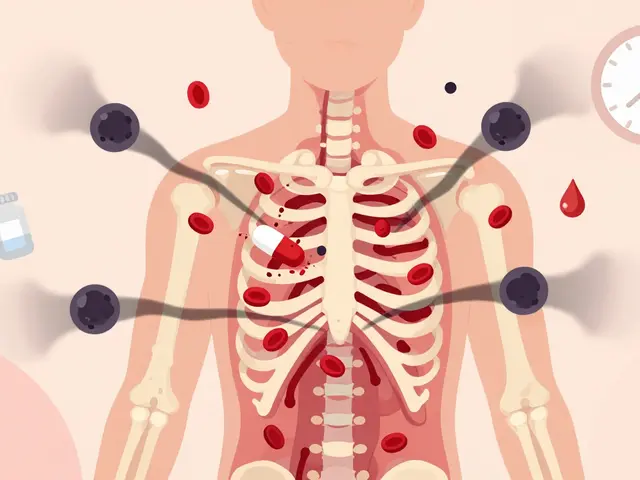
For people who want a lasting solution, Immunotherapy, a series of allergy shots or tablets that gradually desensitize the immune system to specific allergens can change the game. It’s a commitment—typically a few years of regular treatment—but many report a dramatic drop in medication need and symptom severity. In essence, immunotherapy influences allergic rhinitis by retraining the immune response, turning a chronic irritant into a tolerable exposure.
Practical Tips to Reduce Flare‑Ups
Beyond meds, simple lifestyle tweaks keep the nasal passages calm. Keep windows closed on high‑pollen days, use HEPA filters, and shower after outdoor activities to wash pollen off skin and hair. Nasal irrigation with saline solution clears mucus and reduces irritants, making sprays more effective. If you’re prone to eye allergies, antihistamine eye drops can prevent the uncomfortable itching that often accompanies a runny nose.
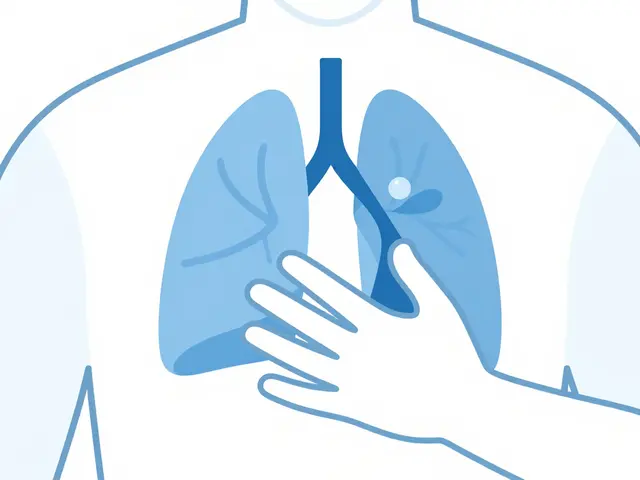
When symptoms overlap with asthma, a combined inhaler that tackles both airway constriction and nasal inflammation may be prescribed. This reflects the close link between allergic rhinitis and lower‑respiratory issues—a fact that underscores why a holistic approach works best.
All these pieces—triggers, related conditions, medication classes, and lifestyle habits—form a network that, when understood, lets you manage the condition with confidence. Below you’ll find a curated collection of articles that dive deeper into each topic, from how specific antihistamines compare to the latest research on immunotherapy protocols. Explore the resources and pick the tips that match your situation, whether you’re seeking quick relief or a long‑term plan.
Sneezing and Your Sense of Smell: Understanding the Link
Discover why sneezing can affect your sense of smell, the conditions that link them, warning signs, and practical tips to keep your olfactory health intact.