Blood Cancer: What You Need to Know
Blood cancer isn’t one disease – it’s a group of cancers that start in the blood‑forming tissue, like bone marrow, or in the cells that travel through your bloodstream. The three big categories are leukemia, lymphoma and multiple myeloma. Each one behaves a bit differently, but they all share a common problem: they disturb the way your blood works.
Common Symptoms and When to See a Doctor
Because blood carries everything in your body, the signs of a blood cancer can feel vague at first. Fatigue that won’t go away, easy bruising, frequent infections, and unexplained weight loss are classic red flags. Some people notice swollen lymph nodes, especially in the neck or armpits, while others feel bone pain or notice a feeling of fullness in the abdomen.
If you have any of these symptoms for more than a few weeks, it’s worth talking to a doctor. Early detection can make treatment smoother and improve outcomes.
Diagnosis and Treatment Basics
Doctors start with a blood test to check for abnormal cell counts. If something looks off, they may order a bone‑marrow biopsy or imaging scans to see where the cancer is hiding. The exact diagnosis – whether it’s acute or chronic leukemia, Hodgkin or non‑Hodgkin lymphoma, or myeloma – guides the treatment plan.
Treatment options have grown a lot in the past decade. Chemotherapy is still common, but targeted therapies, immunotherapy and stem‑cell transplants are now standard for many patients. The right mix depends on the cancer type, stage, age and overall health.
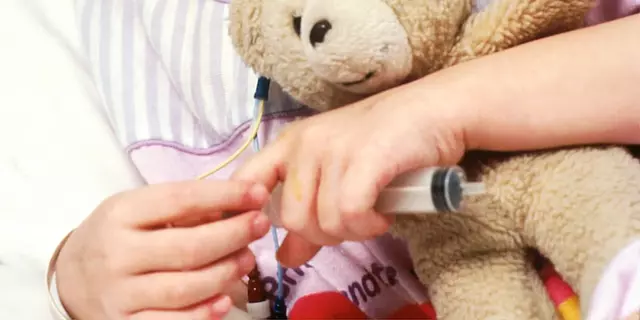
For example, acute lymphoblastic leukemia (ALL) in children often uses a combination of chemotherapy and a bone‑marrow transplant, leading to cure rates above 80%. Meanwhile, chronic lymphocytic leukemia (CLL) in older adults may be managed with oral targeted drugs that have fewer side effects.
Lymphoma treatment varies too. Early‑stage Hodgkin lymphoma can be cured with just a few rounds of chemo and radiation. Advanced non‑Hodgkin lymphoma may need a longer chemo regimen plus newer agents like CAR‑T cell therapy, which re‑programs a patient’s own immune cells to attack the cancer.
Multiple myeloma, the cancer of plasma cells, is now treated with a three‑drug backbone: a proteasome inhibitor, an immunomodulatory drug, and a steroid. Adding a monoclonal antibody can extend survival even further.
Supportive care matters just as much as the drugs. Blood transfusions, antibiotics for infections, and growth factors to boost white‑blood cells keep patients feeling better during treatment. Nutrition counseling and mental‑health support also help manage the stress that comes with a cancer diagnosis.
Every blood‑cancer case is unique, so it’s crucial to work with a hematology‑oncology team that can tailor the plan to you. Ask about clinical trials – many cutting‑edge therapies start there, and participation can give access to the latest treatments.
Bottom line: blood cancer can be scary, but the medical community now has a wide toolbox of therapies. Knowing the signs, getting tested early, and staying informed about treatment options give you the best chance for a positive outcome.
Why Blood Cancer Awareness and Advocacy Matter: A Comprehensive Guide
Learn why blood cancer awareness saves lives, how advocacy fuels research, early warning signs, and practical ways to get involved with reliable resources.