SGLT2 Inhibitors: What You Need to Know
When working with SGLT2 inhibitors, a class of oral drugs that block the sodium‑glucose co‑transporter‑2 in the kidneys, causing excess glucose to be expelled in urine. Also known as gliflozins, they have moved from niche diabetes pills to essential tools for managing type 2 diabetes, a chronic condition marked by insulin resistance and high blood sugar, heart failure, a syndrome where the heart cannot pump enough blood to meet the body’s needs and chronic kidney disease, progressive loss of kidney function over time. In plain terms, SGLT2 inhibitors lower blood glucose, reduce the risk of heart‑failure hospitalizations, and slow kidney decline – a triple win for many patients. This combination of effects makes the class a unique bridge between endocrinology and cardiology, and explains why guidelines now list them alongside traditional blood‑pressure and cholesterol medicines.
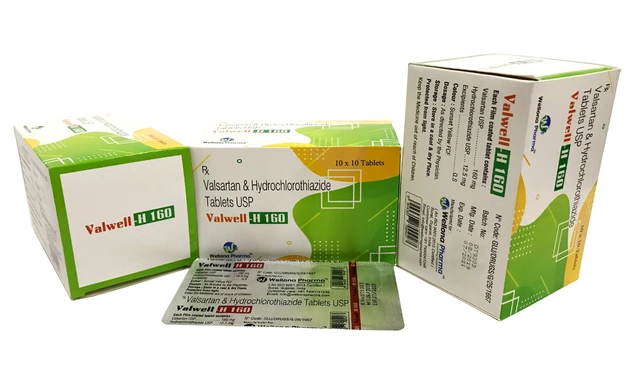
SGLT2 inhibitors come in several brand‑name forms – canagliflozin, dapagliflozin, empagliflozin, and others – each with its own FDA approvals and dosing quirks. Canagliflozin was the first to get a label for reducing major adverse cardiovascular events, while dapagliflozin earned a nod for treating heart failure with reduced ejection fraction, even in patients without diabetes. Empagliflozin stands out for its proven benefit in lowering cardiovascular death. Across the board, the drugs share common side effects: genital yeast infections, urinary tract infections, and a rare but serious risk of euglycemic ketoacidosis. Because they act on the kidneys, they also cause modest reductions in blood pressure and modest weight loss, which can be a pleasant bonus for many users. When you combine an SGLT2 inhibitor with a GLP‑1 receptor agonist or a traditional metformin regimen, you often see synergistic glucose control without a dramatic increase in hypoglycemia risk. However, clinicians must pause the medication in patients with very low eGFR, recent ketoacidosis, or those planning major surgery.
Prescribing SGLT2 inhibitors today means thinking about the whole patient – not just the A1C number. Start with a baseline kidney function test, educate patients on recognizing early signs of ketoacidosis, and schedule follow‑up labs at three‑month intervals. Insurance coverage can be tricky, so checking formulary options early saves time and frustration. Ongoing trials are exploring their role in non‑diabetic populations, such as those with heart failure with preserved ejection fraction and even in obesity management. As the evidence base expands, you’ll see more physicians adding these drugs to the front line of chronic‑disease care. Below, you’ll find a curated list of articles that dive deeper into specific drugs, safety tips, and real‑world prescribing strategies, giving you the tools you need to make informed decisions for your patients.
Medications in Heart Failure: What You Need to Monitor Closely
Heart failure medications like ARNIs, beta-blockers, MRAs, and SGLT2 inhibitors require careful monitoring to avoid dangerous side effects. Learn what to check, when, and how special populations need different care.
SGLT2 Inhibitors and Yeast Infections: What You Need to Know About Urinary Complications
SGLT2 inhibitors help lower blood sugar in type 2 diabetes but increase the risk of yeast and urinary tract infections. Learn how these drugs work, who’s most at risk, and what to do if you develop symptoms.
Empagliflozin vs Alternatives: In‑Depth Comparison
A detailed side‑by‑side look at Empagliflozin versus other diabetes drugs, covering benefits, risks, dosing and how to pick the best option for heart, kidney and weight goals.